At the American Society of Hematology meeting, companies are racing to develop a treatment for SCD, which is an inherited disorder caused by a genetic mutation in the beta-chain of hemoglobin. Some of the data presented by companies were promising, while others reported setbacks.
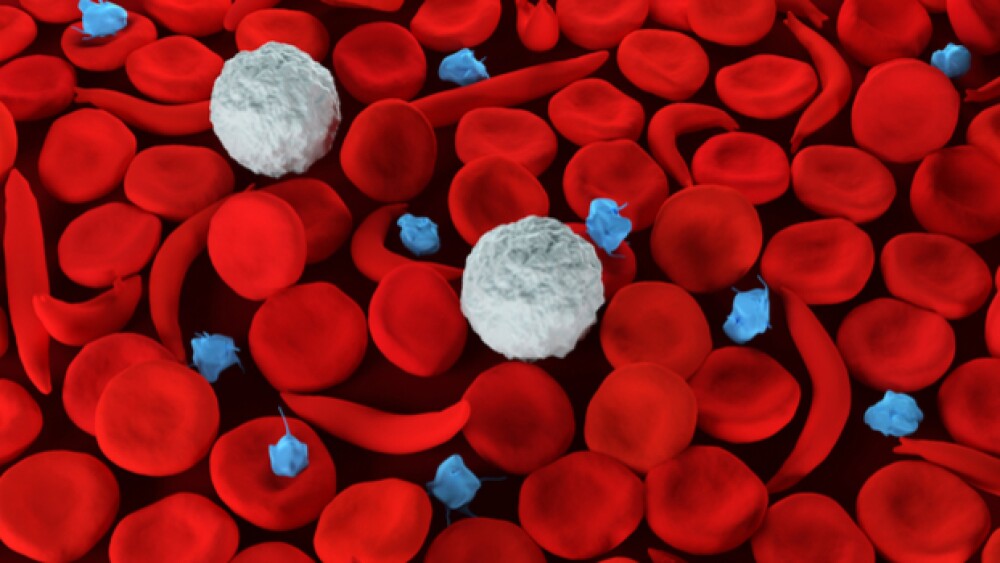
Abnormally-shaped blood cells found in sickle cell disease.
During the annual American Society of Hematology meeting, multiple companies unveiled data as potential treatments for sickle cell disease. Some of the data presented by companies were promising, while other companies reported some setbacks.
Aruvant Sciences, a subsidiary of Roivant Sciences, reported some early positive data regarding its gene therapy treatment for sickle cell disease from an ongoing Phase I/II trial. The company is developing RVT-1801, an investigational gene therapy for sickle cell disease and β-thalassemia. RVT-1801 uses a patented, modified gamma-globulin sequence deliver the gamma-globin gene for production of fetal hemoglobin (HbF) in patients. Aruvant said so far, two patients with sickle cell have been administered treatment with the gene therapy. One year after treatment, the company said both patients continue to exhibit evidence of “sustained, stable, genetically-modified cells in blood and bone marrow” with highly polyclonal markings. Both patients have seen platelet counts increase and both patients show signs of reductions in disease burden, Aruvant said. Additionally, Aruvant said both patients treated with RVT-1801 have had minimal acute toxicity to date.
While Aruvant’s gene therapy has not shown any toxicity issues, bluebird bio noted that one sickle cell disease patient who underwent treatment with its LentiGlobin therapy experienced a setback, but one not likely related to the treatment. A patient who received LentiGlobin about three years ago in a Phase I/II study developed myelodysplasia syndrome, a blood disorder that if untreated can develop into leukemia. Following an analysis of the patient, an independent data monitoring committees, along with the treating physician, agreed the development of myelodysplasia syndrome was unlikely related to LentiGlobin gene therapy. Despite that assurance from the committee, many investors dumped shares of bluebird after the data was released.
bluebird’s data showed that some positive results for sickle cell patients who were treated with LentiGlobin in an ongoing Phase I/II trial. Patients treated with the therapy saw increases in hemoglobin and HAE levels. Also, in all patients who received LentiGlobin treatment, frequency of vaso-occlusive events, which include recurrent pain crises that lead to organ damage and shortened lifespan, was reduced, the company said.
Researchers from St. Jude Children’s Research Hospital also showcased some data for sickle cell disease. According to Eureka Alert, St. Jude researchers “identified the protein UHRF1 in a gene editing-based screen designed to find proteins that facilitate the fetal-to-adult hemoglobin switch.” Mitchell Weiss, chair of the St. Jude Department of Hematology, told Eureka Alert that UHRF1 is the “guardian of methylation throughout the genome.” Methylation is the process for adding or removing methyl groups from DNA, which regulates gene expression, Eureka Alert noted. In the interview, Weiss said the study shows “where methylation is most important for turning off fetal hemoglobin with the goal of reactivating it in individuals with sickle cell disease or beta-thalassemia to alleviate their symptoms.”
Global Blood Therapeutics released data from an interim analysis of its Phase III HOPE study in patients age 12 and older with sickle cell disease that showed patients treated experienced “rapid, robust and sustained improvements in hemoglobin levels and measures of hemolysis with a favorable safety and tolerability profile.”
“These longer-term efficacy and safety data from more than 150 patients enrolled in the HOPE Study continue to support the potential of voxelotor to be a disease-modifying treatment for SCD. These major improvements in anemia and hemolysis have the potential to prevent the chronic organ damage that is the leading cause of death in patients with SCD in the United States,” Elliott Vichinsky, lead investigator of the HOPE Study and Director of Hematology/Oncology at UCSF Benioff Children’s Hospital in Oakland, Calif. said in a statement.
Another data report at ASH shows that children from sub-Saharan Africa who have sickle cell anemia and were treated with the leukemia drug hydroxyurea for six months “demonstrated reductions in sickle-related clinical events, transfusions and rates of malaria and mortality,” Healio reported. According to the report, the benefits of using hydroxyurea to treat the children included “increases in hemoglobin concentration, mean corpuscular volume and fetal hemoglobin.” Additionally, there were decreases in white blood cell count, neutrophils and reticulocytes, Healio reported. Also, the researchers from Centre Hospitalier Monkole in Kinshasa, Congo, reported vaso-occlusive pain, acute chest syndrome and transfusions, were reduced by almost 50 percent.
While companies reported on updates for sickle cell disease treatments, the American Society of Hematology previewed clinical guidelines for disease treatment, with an intent to release a final set of guidelines next year, MedPage reported. According to the report, there are more than 50 recommendations from five sickle cell disease guideline panels. During a meeting over the weekend, the panels discussed key recommendations in the treatment of disease. One example provided by MedPage was that ASH has recommended against “performing routine screening echocardiograms to identify pulmonary hypertension in asymptomatic children and adults with SCD.” The recommendation, the article said citing a panel member, was based on “low-quality evidence.”
Additionally, ASH recommended that new guidelines issued by the American College of Cardiology/American Heart Association on blood pressure should apply to sickle cell disease as well. The panelists said it believes that adopting those blood pressure guidelines will provide a benefit to sickle cell patients.