Facing the looming threat of AMR, researchers finally have a new clue as to why attempts to develop an effective S. aureus vaccine have failed. BioSpace spoke with the team leaders.
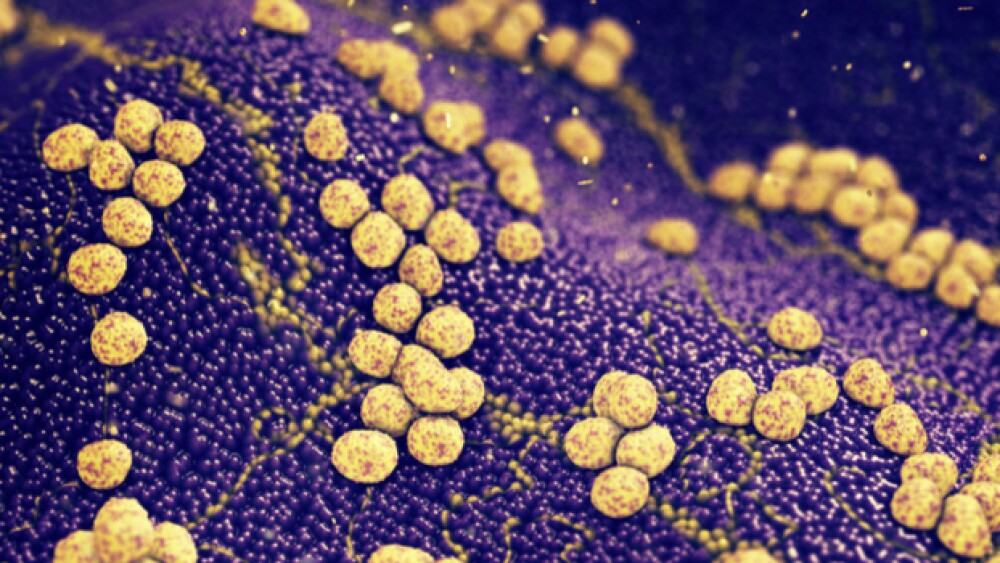
Antibiotic resistance, especially to Staphylococcus aureus (S. aureus), accounted for approximately 1.2 million deaths globally in 2019 and tens of millions of infections. Vaccine developers have tried to address the situation, but have universally failed to translate any effective S. aureus vaccine from mice to humans. Now, however, researchers finally understand why prior attempts failed and - importantly - what they need to do to develop an S. aureus vaccine that is effective in humans.
Targeting the Subdominant Protective Subdomain
“We found that during staph infection, antibodies are generated only to the part of the staph (IsdB) antigen that is not protective. That probably makes sense, since staph is trying to avoid being killed by the host immune system,” lead contact George Liu, M.D., Ph.D., professor of pediatrics at University of California San Diego School of Medicine and chief of the division of infectious diseases at Rady Children’s Hospital-San Diego, told BioSpace.
“We showed that there is a so-called ‘subdominant’ protective domain that does not induce antibody response during staph exposure,” he continued. “If we just vaccinate against that subdominant domain alone, we could induce protection. So, the proposed approach for vaccine developers is to target the subdominant protective subdomain rather than the whole antigen.”
A paper published Thursday in Cell Host & Microbe proposes that the failure of earlier vaccines depended on prior exposure to the pathogen. Liu and colleagues noted that the mice used to test the initial vaccines had little or no exposure to S. aureus before being vaccinated. At that stage, many of the vaccines were effective in mice but failed in humans. Humans, it appears, are exposed to S. aureus very early in life. Half of babies host active colonies and antibodies to fight off infections two months after birth.
Vaccinating babies against S. aureus infections soon after birth doesn’t appear to be a good solution, however. As Liu explained, “Hypothetically, since antibodies are transferred from moms to babies during the last trimester, these non-protective maternal antibodies could compete against newly-formed protective antibodies from vaccination. Therefore, vaccination of babies may lead to a suboptimal outcome...but that will need to be studied.”
The more pressing issue has been the universal failure of staph vaccines in human trials, despite success in preclinical studies.
Impervious Staph Renders Vaccines Ineffective
“Staph vaccines appear so easy to make in laboratory mice because they rarely see S. aureus, but humans are exposed to staph beginning in the first weeks of life and, in order to coexist, staph appears to have developed many strategies to render ineffective our immune response against them,” first author Chih-Ming Tsai, Ph.D., a project scientist in Liu’s lab, said in a statement. “If mice had staph infections before vaccination, we think that the vaccine candidates might not work.”
Liu, Tsai and team tested this hypothesis by simulating one of the largest failed staph vaccine trials in humans, which targeted the IsdB protein used by S. aureus to acquire the iron it needs to function.
They found – not surprisingly – that the vaccine worked in mice who were unexposed to the pathogen, but not in those with prior exposure. The latter only generated antibodies against the unprotected portion of the IsdB protein. Boosters did not remedy the problem. Next, they tried mixing human IsdB antibodies with protective antibodies made from the vaccine. Those protective antibodies became ineffective.
Therefore, the researchers vaccinated mice only against the protective component of the IsdB protein. In that situation, the mice were protected against infection even if they had been previously exposed to S. aureus. The researchers concluded that the earlier vaccines failed because of the faulty memory of the pathogen and the corresponding immune response.
Next Steps: Reconfirming the Hypothesis
“Our next aim is to determine if the same principle could explain the failure of all other failed staph vaccines,” Liu told BioSpace. “Based on (this) new understanding of how staph vaccines failed, we could look for new ways to overcome the root cause of vaccine failure in our study - the non-protective memory left by prior staph exposure.”
Other researchers have noted the role of immunological memory in determining the effectiveness of S. aureus vaccines. Omid Teymournejad and Christopher Montgomery, for example, writing last year in Frontiers of Immunology, noted that in humans, a pathogen’s ability to redirect immune responses from the protective antigens precluded the development of natural memory and, therefore, potentially inhibited vaccine efficacy.
A Pressing Concern
Addressing S. aureus infections is a serious concern, especially given the growing resistance to such common treatments as methicillin. In addition to vaccines, other researchers are exploring bacteriophages, monoclonal antibodies, centyrines and new types of antibiotics to prevent or treat S. aureus infections. Perhaps the latest endeavor is the just-announced formation of Aurobac, a joint venture of Evotec SE, Boehringer Ingelheim and bioMérieux, to develop next-generation antimicrobials to combat antimicrobial drug resistance.
Nonetheless, vaccines may well be the most effective way to reduce the health burden of staph infections and simultaneously reduce antibiotic resistance, Liu suggested. He predicted that this research may lead to an effective S. aureus vaccine in the relatively near future, adding, “It is even possible that the same principle also may explain why many other hard-to-make vaccines have failed.”