‘Flatten the Curve’ is sure to become a phrase forever linked with COVID-19. It refers to doing all we can as individuals to slow the spread of COVID-19 so that all available resources can be used for those who need them most urgently.
‘Flatten the Curve’ is sure to become a phrase forever linked with COVID-19. It refers to doing all we can as individuals to slow the spread of COVID-19 so that all available resources can be used for those who need them most urgently. On Friday, experts Dr. Scott Gottlieb and Dr. Paul Biddinger explained in a webinar co-hosted by WIRB-Copernicus Group (WCG) and Accumen that the rapid spread of the virus is one of the greatest threats to those at greatest risk of severe or deadly complications.
Why Does the Rate of Spread Matter?
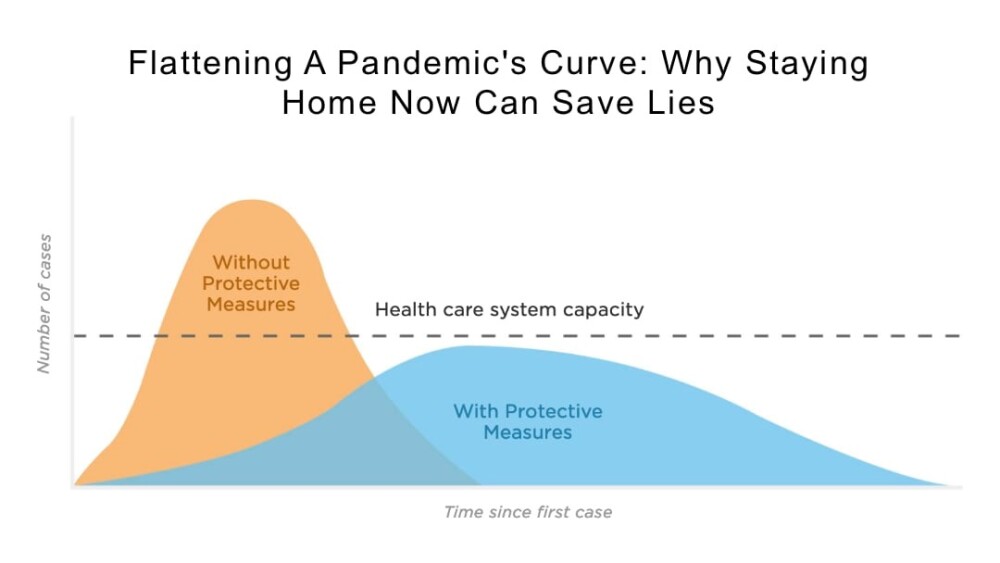
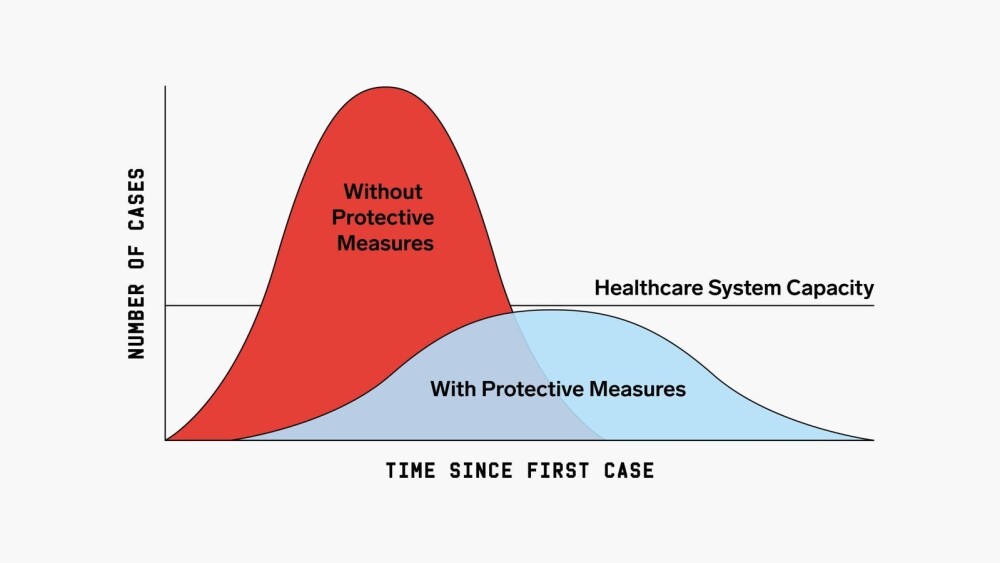
The rate of spread – how quickly the virus is infecting new people – determines the number of patients entering the healthcare system at the same time. If the virus is spreading rapidly, many people will enter and need resources ranging from a test to time in the ICU within a very short timeframe. As with nearly anything else, if more people require attention than it is possible for those meeting the need to deliver, the system will be overwhelmed and there will not be enough capacity for everyone. In the case of COVID-19, those at lowest risk may not require any attention at all. Those at greatest risk will require extensive, specialized attention.
Dr. Biddinger of Massachusetts General Hospital (Chief, Division of Emergency Preparedness and Director, Center for Disaster Medicine) provided this assessment with the rationale for working to flatten the curve: “I don’t think it’s possible to put the Genie back in the bottle. I think we’re going to continue to see rising numbers of cases, and I think a lot of our efforts, maybe all of our efforts, are focused at blunting the epidemic curve. Keeping the peak as low as possible because that peak is where the medical demands potentially exceed capacity. The higher that peak, the more people we may see who need hospitalization, who need intensive care, who need resources like a ventilator or ECMO, which is a version of bypass to help support oxygenation. The higher the peak, the more we can’t provide these kinds of resources.”
Source: CDC, Drew Harris
Credit: Connie Hanzhang Jin/NPR
Why Limit Social Contact?
One way to slow the rate of spread and flatten the curve is to keep people apart. The idea behind social distancing is just that and social distancing is proving especially important with COVID-19 because we are seeing increasing rates of community transmission. In the case of community transmission someone will contract the virus from someone in the community – someone who did not travel or engage in anything that would expose them to the virus. The rising rate of community transmission is indicative of the fact that, “the disease is clearly spread by both asymptomatic individuals as well as by individuals before they begin to feel ill,” said Dr. Biddinger, “which is a characteristic of influenza. That makes this much more difficult – I would argue impossible – to control with public health measures [identification and isolation] directly. Once the disease is in the community, especially because of the minimally symptomatic or asymptomatic spread but also because transmission can happen before patients have symptoms, it really takes root.”
The fewer opportunities there are for people to mingle with others, the less likely it will be that new cases of COVID-19 occur.
Source: CDC, Drew Harris
Credit: Connie Hanzhang Jin/NPR
What’s Next?
One essential consideration is to keep the workforce of healthcare workers healthy and available. In our current situation, physician’s offices and Emergency Rooms are dealing with questions and concerns from a wide range of people. There are also people who need to be tested. “Our testing strategies for broad-based public testing have to be much more thoughtful. People have seen drive-through testing clinics and others that don’t bring the well and the ill together and don’t overwhelm the care system,” said Biddinger. “Those are the things we really need to look at. On the ambulatory care side, it’s important to talk about how challenging COVID-19 is.”
Up until now, testing has been limited but important. The importance has been in knowing where the virus is. As it becomes more widespread, there will be fewer instances in which a test will provide anything useful. This is especially true with young, healthy individuals. For the majority of these, COVID-19 will be the equivalent of a nasty case of the flu. They won’t require hospitalization and, since there is no treatment, will not require formalized medical care unless their symptoms worsen.
Dr. Biddinger explained that flattening the curve may mean that COVID-19 will be active for “somewhat longer” than it might have been had it spread without mitigation. The thing to remember is that we are not working to stop the virus before it’s run its course. We are working to slow the rate of transmission – to flatten the curve – so that the medical community can meet the needs of those who most urgently require that care.
Bottom Line
The validity, and urgency, of efforts to mitigate the spread of COVID-19 is not subjective: In a situation where resources – the equipment required to protect healthcare workers, provide necessities like respirators to those with the most severe cases, and ensure space in the ICU for those in dire condition – are not limitless, the only way to protect everyone effectively is to allocate those resources carefully. If we as individuals can use social distancing to slow the rate of transmission to avoid spiking the curve and overwhelming our healthcare system, we will come through this with a far greater number of good outcomes.
Want to hear this for yourself? COVID-19 Preparedness: Information from Experts, co-hosted by WIRB-Copernicus Group (WCG) and Accumen.
Other Resources:
World Health Organization (WHO) Q&A on Coronaviruses (COVID-19)
NPR – Why Staying Home Saves Lives
Please click here for more information on our contributing writer, Gina Hagler.