Before next-generation metabolomics becomes mainstream, the medical establishment needs to expand its mindset around cancer and translate this understanding into the clinic.
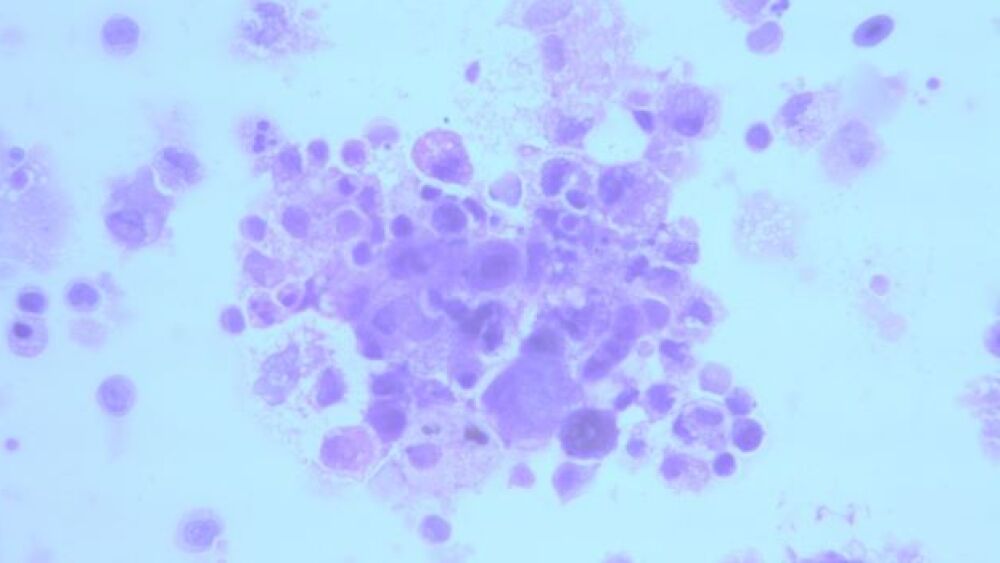
A close-up of dying cancer cells/courtesy of Metabolomycs, Inc.
Next-generation metabolomics has proven its scientific value. Before it becomes mainstream, however, the medical establishment needs to expand its mindset around cancer and then improve ways to translate this understanding into the clinic.
“In the early 2000s, Janet Woodcock suggested that the healthcare establishment had devoted too much effort towards developing drugs, and not enough effort toward connecting good ideas to utility,” Robert A. Nagourney, M.D., founder of the Nagourney Cancer Institute and of Metabolomycs, Inc., told BioSpace.
More recently, President Joe Biden’s February 2 address reignited the Cancer Moonshot he launched as vice president under President Barack Obama. This new phase calls for identifying better ways to target the right treatments to the right patients. “We understand too little about why treatments work for some patients, but not for others,” he said.
In practice, that means recognizing that genomics is only the starting point in discovering and developing patient therapies. “Genomic profiles are like satellite maps,” Nagourney said. “They may tell you that a gene is present in the disease process, but not whether it is the driver of disease or is just a passenger.” Ex vivo cell analysis combined with next-generation metabolomics can provide that insight.
As Nagourney elaborated, a genomic test that identifies a target mutation or amplification is just the starting point in understanding cancer biology. “The most common gene implicated in cancer is p53. About half of cancer patients have this abnormality, but its presence or absence doesn’t tell physicians what to do. Drugs under development for treating this p53-associated cancer often have nothing in common with one another. Our best efforts to treat cancer genomically are failing.
“Likewise, the oncogene Myc regulates 3,600 separate genes and is responsible for 15% of all genomic regulation in the human body. It’s abnormally active in up to 70% of all human cancers, and yet it is almost never mutated,” Nagourney pointed out. By focusing so heavily on genomics in cancer, “we’re answering questions no one asks. Patients want to know how to get better, but their physicians are responding by telling them that their cancers are associated with the presence of Myc, or p53 or K-Ras. In effect, they’re saying ‘we don’t have a treatment, but we know all about you.’”
Nagourney’s labs are interested in the study of the cellular response within human tumors, as opposed to studying the genes or proteins implicated in a specific cancer. “Looking at analytes can’t tell you whether drugs will be synergistic until you put them together,” Nagourney said.
Nagourney’s ex vivo cellular analysis approach, dubbed an explant, addresses that challenge. These explants have the actual tissue architecture of the tumor in its native state, including the stroma, cell-to-cell communications, cytokines… “the whole gemish that makes up a tumor,” he said.
This avoids the issues associated with studies using organoids, which don’t accurately replicate the tumor. As Nagourney explained, “Organoids start with one cell and propagate it, but most cancers in the body have relatively low proliferation rates, often less than 15%.” The act of growing tumor cells perturbs the system, thus skewing the results.
The study of cancer also suffers from an incomplete understanding of the disease. “Cancer, as a disease, is not a cell growth abnormality, but a cell survival abnormality. It’s a group of cells that don’t die,” he said. Treating cancer as a cell proliferative condition by studying a treatment’s effect upon DNA synthesis or cell mitosis often results in false positives.
“But, if cancer is a cell survival problem, the only way to measure whether a therapy works is to kill the cancer cell,” Nagourney said. For example, rather than focusing upon apoptosis, his ex vivo model of programmed cell death incorporates all mechanisms implicated in cell death, including apoptosis, necroptosis, ferroptosis, PARP-mediated cell death, calcium flux-mediated cell death and other forms. The result is a more predictive model that he can use when testing therapeutic combinations. His labs maintain a library of 150 small molecules targeting known pathways of cancer.
Cancer involves more than just its genetic elements, Nagourney stressed. He said that focusing on its genetics is like viewing a satellite map of greater Los Angeles. “There are many different arteries running into the city. Looking at it would tell you how to get from point A to point B. But the last thing you would want is to use a static map to drive there when what you need is a dynamic map with real-time traffic information.” The recent L.A. Super bowl traffic patterns underscore the value of real-time information in that example. Functional biological analysis, available through ex vivo cellular analysis, provides real-time insights into cancer.
The point, he said, is to identify the best therapeutic option for patients quickly. That wasn’t particularly difficult when cancer therapies were limited to five or six drugs. That landscape has changed dramatically in the past several decades.
In 2021 alone, the FDA approved 16 therapeutics for various cancers. That means there are ever-increasing possibilities of combinations. Having a way to assess the therapeutic value of such combinations will be increasingly valuable.
“As a pharmacologist, I see drugs in terms of mechanisms of action,” Nagourney said. “By examining those mechanisms, I see how drugs interact and can test them,” using the ex vivo cellular assay he developed. “Now, a large number of scientists around the world are interested in cellular testing, but it’s not a trivial undertaking.
“The problem in cancer research is that we tend to be reductionists, and cancer is extremely complex, so it doesn’t play ball,” he said. Gene profiles are a good start – but are only a start. The question is whether a gene is a driver or a passenger. Functional capability studies can answer that.”