NKarta Therapeutics is using engineered chimeric antigen receptor natural killer cells (CAR-NK cells) for allogeneic therapy, showing substantial benefits both in vitro and in vivo, according to James Trager, CSO, speaking Wednesday at the virtual CAR-TCR Summit – Europe.
NKarta Therapeutics is using engineered chimeric antigen receptor natural killer cells (CAR-NK cells) for allogeneic therapy, showing substantial benefits both in vitro and in vivo, according to James Trager, CSO, speaking Wednesday at the virtual CAR-TCR Summit – Europe.
Specifically, one of NKarta’s two lead compounds, NKX019, “showed robust activity, longer half-life than non-engineered NK cells, faster onset of activity, and the production of fewer cytokines than CAR T cells. A first-in-human trial of NKX019 in B cell malignancies is planned for 2H 2021,” Trager said.
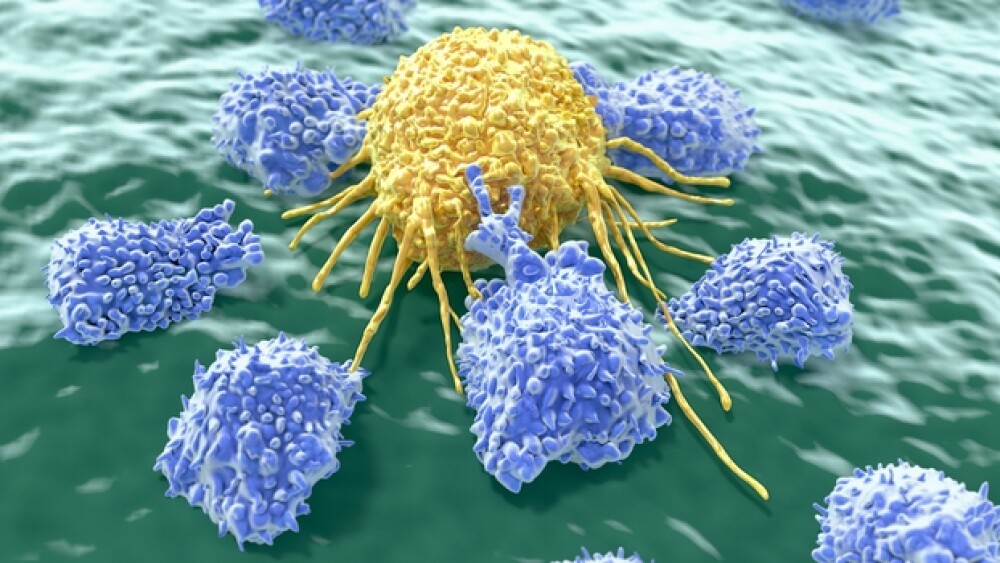
“Natural killer cells are the cornerstone of innate immune surveillance,” Trager said. They offer allogeneic, “off-the-shelf” accessibility.
NKarta’s engineering enhances their persistence and tumor targeting.
“They are more potent when used allogeneically, and can be scaled to a large degree. They also can be cryopreserved, which lowers the cost of manufacturing,” Trager said.
The company’s engineered NK cell program is based on four core technologies. For expansion, the program co-cultures cells with a stimulatory cell line to achieves high doses. Persistence is achieved by expressing membrane-bound IL-15 (mbIL15). For tight targeting, the cells are engineered to express optimized CARs.
“Researchers can put on different targeting heads to change the tropism of the cells,” Trager said.
Cryopreservation, the fourth technology, exacts no toll on the cells. Their effectiveness matches that of non-cryopreserved cells.
Notably, NKarta expands the cells before transducing them.
“This puts the expensive part of the process up front,” he explained. “Efficacy is much greater when cells are in a robustly proliferatively state, so the expansion and retroviral engineering occur during the first few days.” Although such early expansion is not necessarily easy to achieve, “working with small cell numbers lowers cost of goods.”
“After that, we’re expanding in a bioreactor,” he continued, where continued expansion is driven by the expression of mbIL-15.
This approach drives large-scale manufacturing, enabling NK cells to be expanded more than 1,000-fold (including viral transduction) in two weeks. Trager shared a chart showing the expansion level at 3,364 cells after 15 days. Projected cost estimates for commercial manufacturing, at 500 doses per batch, are approximately $2,000 per dose.
“That’s very competitive in the cell therapy field,” Trager said.
“A lot of work goes into this,” he pointed out, discussing NK cell engineering. “NK cells, even before we engineer them, provide initial control over tumor cells, but they lose control after a couple of challenges.”
NKarta’s engineered, but-not-yet optimized CAR NK cells, in contrast, can withstand six to seven challenges. Optimized CAR-NK cells withstood more than seven challenges by tumor cells.
“Cryopreservation is difficult to achieve while maintaining potency,” Trager noted, but NKarta seems to have succeeded. In a chart comparing the activity of cryopreserved and thawed CAR-NK cells to fresh and non-engineered NK cells, the differences in activity among fresh cells and three runs of frozen and thawed NKX101 cells were minuscule.
The real difference was between engineered and non-engineered cells. Tumor activity was approximately three-fold lower for fresh and frozen/thawed CAR-NK cells than non-engineered NKs, and approximately six-fold lower than for controls, thus reinforcing the superiority of the engineered cells.
As Trager said, NKX019, a CD-19-targeted CAR NK, provides “stunning potency” and “options for patients the point of need with, possibly, less risk or toxicity.”
Others are reporting beneficial results, too. A trial at MD Anderson Cancer Center (published in the New England Journal of Medicine last year) involving Takeda’s CAR19-NK showed complete responses in more than half of patients with advanced B cell malignancies, and no instances of cytokine release syndrome, graft versus host disease, or neurotoxicity.
NKarta’s studies in mice indicated that cryopreserved NKX019 inhibited tumor activity in lymphoma models, as well as prolonged persistence in tumor-naïve mice. Non-engineered NK cells “have a half-life of about nine days. We can roughly double that with engineering,” Trager elaborated.
The goal of this therapy is to maintain the NK cells’ potency while delivering a large number of cells and to ensure acceptable safety profiles. In the case of NKX019, cytokine generation is one-to-two levels of magnitude lower than with unengineered CAR T cells so, Trager surmised, “there’s low risk of triggering cytokine release syndrome.”
Additionally, NKX019 works swiftly, with a faster onset of activity and enhanced potency that combine to kill tumor cells faster than CAR19 T cells.
NKarta also is exploring the synergy between NK and T cells for enhanced potency. “When we combine the two cell types, we see greater potency, and additive activity… that is greater than the sum of the individual components,” he said.
That synergy between NK and T cells stimulated NK cell proliferation and depressed – but did not halt – T cell proliferation. Furthermore, combining CAR19-NK and CAR19-T cells lowered the accumulation of cytokines associated with cytokine release syndrome. “NK cells act as a sink for cytokines,” Trager pointed out.
In mouse models, “The NK or T cells provided limited control but, when combined, survival extended to four months (and in one mouse, six months) before dying of natural causes.
NKarta is eager to learn, later this year, whether such benefits translate to humans.