Detecting the presence of SARS-CoV-2 in asymptomatic individuals has been a challenge not even PCR – the gold standard of testing – can adequately address. Now two companies have developed novel solutions with the sensitivity and specificity needed to provide ample warning.
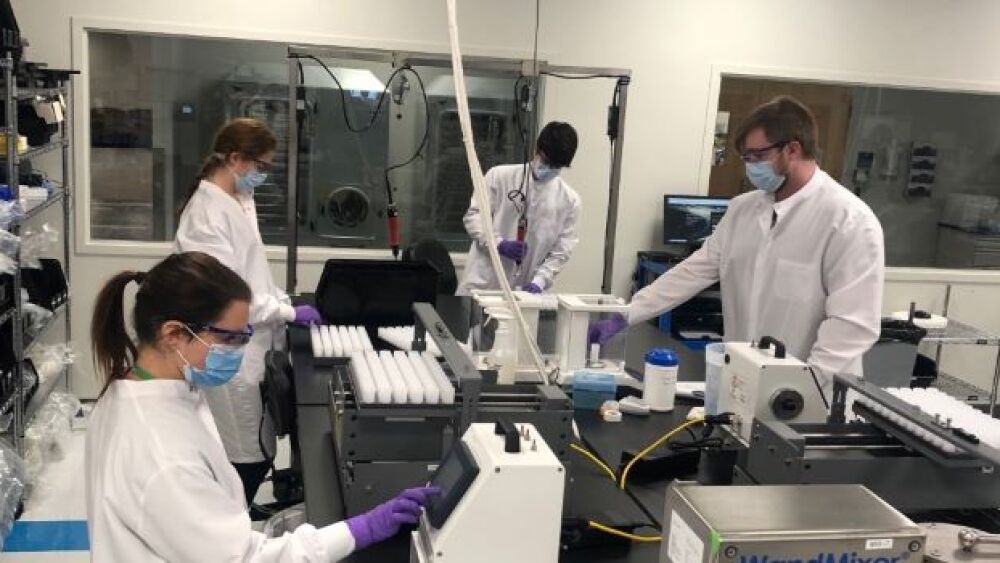
Photo courtesy of Quanterix.
Detecting the presence of SARS-CoV-2 in asymptomatic individuals has been a challenge not even PCR – the gold standard of testing – can adequately address. Now two companies have developed novel solutions with the sensitivity and specificity needed to provide ample warning.
Quanterix is filing Emergency Use Authorizations (EUAs) for assays involving multiple COVID-related biomarkers, based on its Simoa® technology.
“We started with the innate immune system, using cytokines to predict which patients would experience cytokine storms. That assay was used mostly by research hospitals,” Kevin Hrusovsky, Chairman, president, and CEO of Quanterix, told BioSpace.
The second assay measures neurofilament light (NfL), which can indicate neuronal death, for patients who lost their sense of taste or smell, or experienced brain fog.
The most recent assay measures the adaptive immune system.
“Then a private health insurer asked for a serology test to measure the adaptive immune system response using dried blood spots,” Hrusovsky recalled.
Based on that work, the National Institutes of Health (NIH) asked Quanterix to develop an antigen test.
“It provided an $18.2 million contract for scaleup,” Hrusovsky said. “We’re hoping this will be a multi-matrix test to look not just at dried blood samples, but also nasal swabs and saliva.”
The goal is to provide sensitive, specific tests for asymptomatic people. With colleges back in session and some regions of the world allowing tourists to visit (if they have proof of a recent, negative, COVID-19 test), “There’s a lot of asymptomatic screening going on,” Hrusovsky said. Yet, most of the FDA-approved COVID-19 diagnostic tests are for patients experiencing symptoms.
The Quanterix assays fill that void. Because of the extraordinary sensitivity of Quanterix’s technology, the company believes that its assays will be able to detect the virus in its earliest stages, days before symptoms appear.
Consequently, “We might report a positive test result while PCR tests report a negative test result,” he said. “We looked at seven different trials in an effort to clean up the area of false negatives and positives. We found that when you test a person three days before symptoms appear (when virus incubation has started), the PCR false negative rate is about 70%. It can be as high as 95% if you look four to five days before symptoms appear. Thus, PCR tests for asymptomatic people often return inaccurate results that support counterproductive behaviors.”
PCR can register false positives, too.
“After the disease, PCR tests can measure fragments of the virus DNA or RNA weeks or months after the infection. Those fragments remained in the respiratory sample even though the antigen is long gone,” Hrusovsky said.
More accurate testing, therefore, would reduce the number of false positives, allowing former COVID-19 patients to resume their usual activities.
Hrusovsky’s goal is to develop a COVID-19 testing kit for home use. A person could do a finger prick test, “put the sample in an envelope and send it to a central lab via courier. Because Quanterix’s assays have the potential to measure biomarkers in blood or saliva, they are less invasive than assays that require nasopharyngeal swabs.
Quanterix’s newest COVID-19 assay currently is being used as a lab-developed test at CLIA labs pending the FDA’s consideration of the company’s EUA application.
“We have many university labs asking for access to our technology because of its analytical sensitivity,” Hrusovsky said.
Mirimus Labs takes a different approach: pooled testing.
“Tests are a snapshot in time, so people need repetitive testing,” CEO Prem Premsrirut said, speaking on a panel with Hrusovsky at The Contagion Conference. PCR testing was too expensive and pharyngeal nasal swabs were too uncomfortable. To support weekly, low-cost testing for schools and workplaces, it developed SalivaClear™, an RT-PCR assay.
The system uses a 2mL sterile tube and a straw, into which a person deposits 1mL of saliva.
“Testing saliva is just as sensitive as (testing) pharyngeal nasal swabs, but can be done comfortably without needing personal protective equipment or exposing others to the virus,” Premsrirut said.
“This is not random pooling,” she emphasized. Saliva is pooled into classroom or workgroup batches of up to 24 samples for processing. If a test is positive, further testing is performed to identify the infected individual(s).
“Infections occur in clusters, among people who interact with each other,” Premsrirut pointed out. With pooled testing, therefore, contract tracing is half done because if someone in their cluster is infected, they realize they also have had exposure.
Weekly testing allows changes in test results to be measured, allowing infections to be inferred. As she explained, “If a person tested negative last week and is inconclusive this week, we can assume they are in the early stage of infection and will become positive within a day or so.”
Consequently, the test can identify people very early in the disease cycle.
Rapid, non-invasive diagnostic testing is an integral pillar – alongside effective vaccines and therapeutics – in limiting the spread of COVID-19.
“People say, ‘Follow the science,’ but we don’t know what the science is teaching us,” Hrusovsky pointed out during The Contagion Conference. “Vaccines are the next wave of opportunity to manage this pandemic, but there are a lot of unknowns. Are vaccines working? What’s their duration? Getting back to work and being productive is as important for mental health as for economic health. Testing will play a vital role in enabling that.”