The collaboration will focus on expanding the use of 3D bioprinted stem cell-based therapeutic tissues. The goal is to develop treatments for end-stage renal disease.
San Diego-based Organovo announced it is entering a collaboration agreement with Melissa Little at the Murdoch Children’s Research Institute (MCRI), The Royal Children’s Hospital, in Melbourne, Australia, and Ton Rabelink at Universiteit Leiden (LUMC) in Leiden, Netherlands. The collaboration will focus on expanding the use of 3D bioprinted stem cell-based therapeutic tissues. The goal is to develop treatments for end-stage renal disease.
Bioprinting is a type of 3D printing, sometimes called “additive manufacturing.” 3D printing is a way of making three-dimensional solid objects from a digital file. The limitations of what can be printed are seemingly limited only by the complexity of the design. Bioprinting is another application, where instead of using carbon fiber as a source material, it uses biological source materials.
The collaboration will utilize Organovo’s bioprinting platform, MCRI’s advanced stem cell differentiation technology, and LUMC’s cell lines and clinical expertise. The partnership is funded by Stem Cells Australia and CSL Limited.
“Partnerships with world-class institutions can accelerate groundbreaking work in finding cures for critical unmet disease needs and the development of implantable therapeutic tissues,” stated Taylor J. Crouch, chief executive officer of Organovo. “This collaboration is another important step in this direction. With the devoted support of Stem Cells Australia and CSL Limited, leading researchers are able to leverage Organovo’s powerful bioprinting technology platform to achieve significant breakthroughs.”
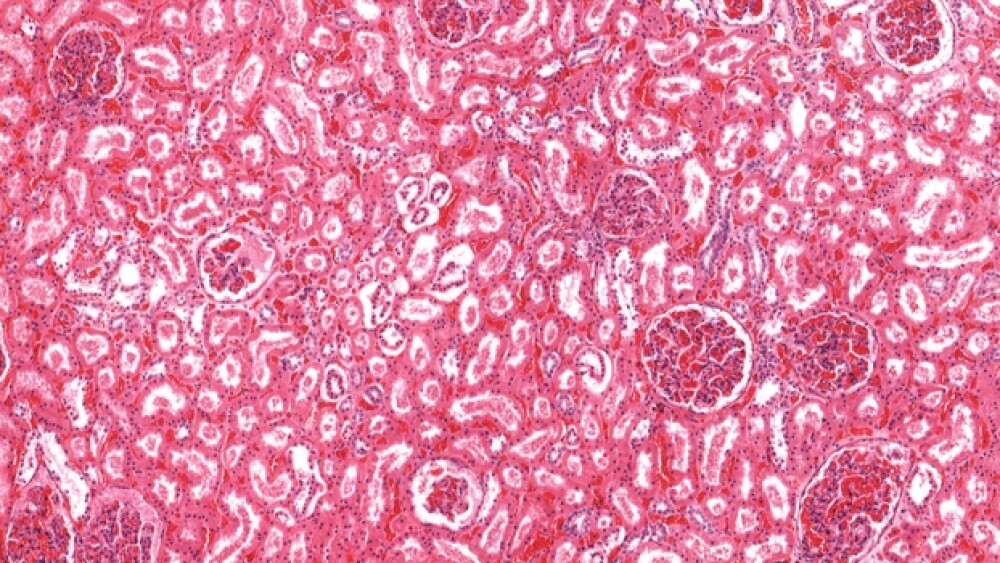
Little, who is Theme Director of Cell Biology at MCRI, notes her proprietary approach for modeling human kidney tissue from stem cells. “By using Organovo’s bioprinter, we can create a stem-cell based therapeutic tissue that may serve as an important step in treating kidney disease.”
This collaboration isn’t the first into human tissue bioprinting. In 2018, Pessac, based in France, along with Prometheus, a division of Skeletal Tissue Engineering in Belgium, inked a two-year Collaborative Research Agreement to develop high-precision 3D Bioprinting of tissue engineered Advanced Therapeutic Medicinal Products (ATMPs) for skeletal regeneration.
Essentially, they are working to “print” bone that can be used in transplants or other orthopedic, musculoskeletal or spine-related applications.
Another company, Poietis, has a product on the market called Poieskin, a human full-thickness skin model produced entirely by 3D bioprinting. The company says it is made up of a “dermal compartment composed of primary human fibroblasts embedded in a collagen I matrix overlaid by a stratified epidermis derived from primary human keratinocytes.”
Poietis also has a deal with L’Oreal to produce synthetic hair follicles.
In 2017, Organovo awarded its 2017 ExVive 3D Tissue Application Award to researchers at Amgen and Medikine. The award is designed to simulate new applications for Organovo’s ExVive Liver and Kidney Tissue.
Earlier this year, researchers at Tel Aviv University successfully printed the first 3D human heart. They used the patient’s own cells and various biological materials such as collagen and glycoprotein. The heart is small but is a fully bioengineered and bioprinted human heart. It’s not ready for human transplantation, but it is a dramatic breakthrough and technological achievement.
Of the collaboration between Organovo, MCRI and LUMC, Christine Wells, deputy program lead at Stem Cells Australia, stated, “The goals of the program are to link experts in bioengineering, stem cell biology and clinical research to address therapeutic gaps in areas of critical unmet need.”