Recently published data from a mouse model of sickle cell disease (SCD) is bolstering the case for the safety of Cell Source’s CD8+ veto cells, currently in Phase I/II testing to improve peripheral blood stem cell transplantation in patients with hematological malignancies.
Recently published data from a mouse model of sickle cell disease (SCD) is bolstering the case for the safety of Cell Source’s CD8+ veto cells, currently in Phase I/II testing to improve peripheral blood stem cell transplantation in patients with hematological malignancies. The paper was published in Bone Marrow Transplantation.
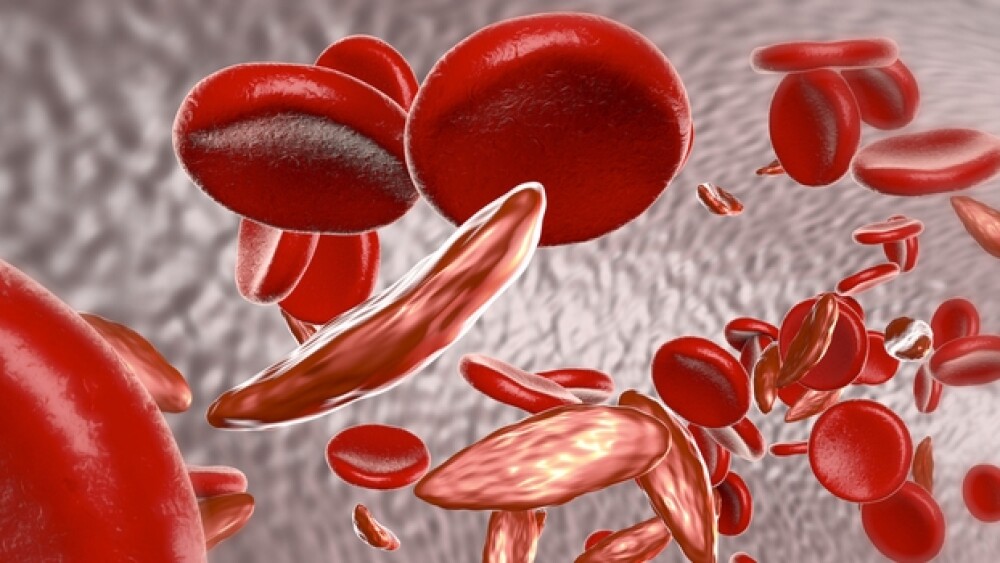
Veto cells are a naturally occurring T cell subtype that block other T cells from an immune response. Cell Source is exploring veto cells as immune suppressors to be given with bone marrow transplantation to prevent T cell-induced graft-versus-host disease, even with mismatched donors and patients, intended as a safer alternative to radiation and chemotherapy.
In blood cancers, aside from its clinical trial, the company is also exploring the cells preclinically in conjunction with chimeric antigen receptor-T cells. Cell Source also has preclinical programs for veto cells for kidney transplants, sickle cell anemia, and type 1 diabetes.
In the paper, University of Texas MD Anderson Cancer Center researchers led by Yair Reisner–who is also chair of Cell Source’s Scientific Advisory Board–selectively depleted populations of CD8+ T cells of anti-host T cell clones, then treated the cells with the cytokine IL15 to expand the population.
In a model of SCD, mice receiving veto cells and rapamycin along with transplanted allogeneic hematopoietic stem cells (HSCs) from mismatched donors had successful engraftment and conversion to normal donor-derived red blood cells, without intensive immune conditioning that can be toxic.
Patients with SCD are treated for symptoms including pain, but companies and clinicians are exploring curative options. Children with severe SCD can receive a donor-matched bone marrow transplant, but the option isn’t available for adults. According to Dennis Brown, Chairman of Cell Source, “Sickle cell disease diminishes the quality of life and lowers the life expectancy of approximately 100,000 people in the United States alone.”
Companies including bluebird bio are exploring one—and-done gene therapies for SCD, but the path has not been smooth. In February bluebird was forced by the U.S. Food & Drug Administration (FDA) into a clinical hold for a Phase I/II study of its LentiGlobin gene therapy when patients developed acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) following treatment. The company said this week an internal analysis indicates its lentiviral vector was not likely to have been the cause of the AML, and it intends to resume clinical studies following regulatory agreement.
Another approach is genome editing. In January, FDA cleared Editas Medicine’s clinical trial for a CRISPR-Cas12a ex vivo genome editing therapy, EDIT-301, in patients with SCD. But ex vivo transplant approaches may still require chemotherapy and radiation. Yesterday, Intellia Therapeutics presented preclinical data from an in vivo proof-of-concept genome editing technique for bone marrow and HSCs in mice. John Leonard, Intellia’s president and chief executive officer, said the data showed it is possible to deliver safer solutions for blood disorders like SCD.
Cell Source’s clinical trial is testing veto cells with transplanted HSCs in up to 24 patients with hematologic malignancies following chemotherapy and radiation. The primary endpoint is a reduction in graft-versus-host disease at 42 days post-transplant.