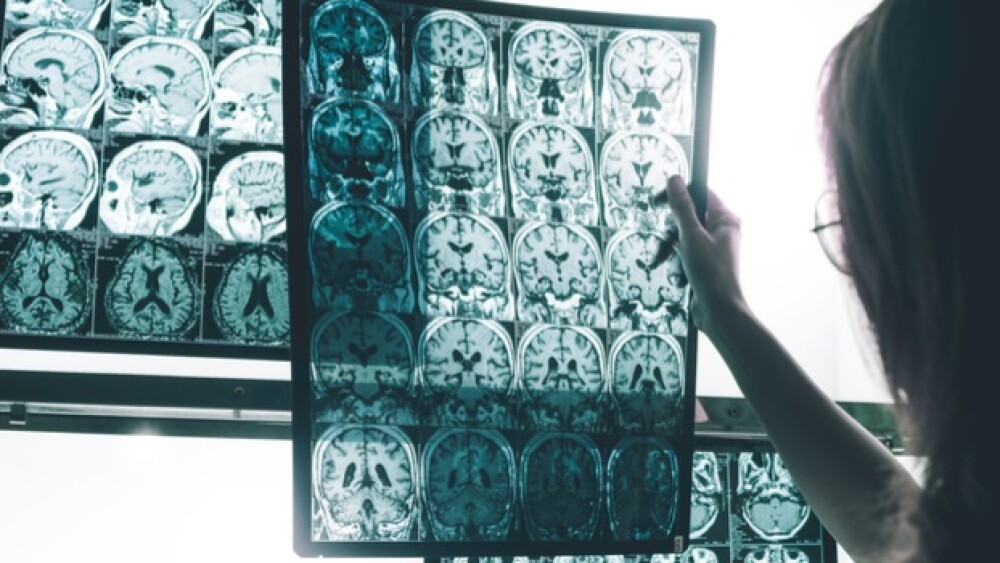
Researchers at Temple University Health System have shown that a type of energy malfunction, called mitochondrial calcium transport remodeling, is involved in the progression of Alzheimer’s disease.
For the last several decades, the dominant theory of Alzheimer’s disease was that it was caused by the accumulation of a protein, beta-amyloid, in the brain. However, failed clinical trial after failed clinical trial suggested that either this theory was just plain wrong or incomplete, that there was something else at work. Some researchers believe that a certain type of energy malfunction, particularly related to immune cells in the brain, is a promising theory—and that beta-amyloid and another protein, tau, is still part of the process.
Researchers at Temple University Health System have shown that a type of energy malfunction, called mitochondrial calcium transport remodeling, is involved in the progression of Alzheimer’s disease. This is a mechanism where cells attempt to compensate for decreased energy production and metabolic dysfunction. Initially helpful, this mechanism begins to malfunction, causing drops in mitochondrial function—part of each cell’s energy production system—memory, and cognition. The research was published in the journal Nature Communications.
Problems with calcium regulation and metabolic dysfunction have been associated with Alzheimer’s development and malfunctioning neurons for some time. Intracellular calcium signaling plays an essential role in synaptic transmission and brain cell communication.
“But up to now, no one has investigated the impact of altered calcium transport into and out of the mitochondria on the progression of Alzheimer’s disease,” stated John W. Elrod, associate professor in the Center for Translational Medicine at the Lewis Katz School of Medicine at Temple University (LKSOM) and senior investigator of the research. “Our current study provides a missing link between these two hypotheses of Alzheimer’s pathogenesis.”
One of the most significant regulators of mitochondrial calcium transport is a protein called NCLX. Elrod’s laboratory previously discovered that NCLX mediated calcium efflux (flowing out) from heart cells. But NCLX expression is vital in mitochondrial calcium efflux in neurons.
Elrod and his team studied a mouse model of mitochondrial calcium uptake by neurons in Alzheimer’s disease. The mice had three gene mutations that lead to age-progressive pathology comparable to Alzheimer’s progression in humans. As the mice aged, they saw a steady decrease in protein expression that limited mitochondrial calcium uptake. This resulted in calcium overload, which damaged the cells. This loss of NCLX also seemed to increase the production of oxidants, further damaging the cells.
When the researchers completely eliminated NCLX expression in the forebrain of Alzheimer’s disease mice, they showed significant memory and cognitive impairment. And this led to significant development of beta-amyloid and tau pathology. When NCLX expression was restored, the beta-amyloid and tau clumps decreased, and neuronal mitochondrial calcium levels were reestablished. The cognitive decline stopped.
“Our findings indicate that maladaptive remodeling of pathways to compensate for abnormalities in calcium regulation, which perhaps are meant to maintain energy production in cells, lead to neuronal dysfunction and Alzheimer’s pathology,” Elrod said. “Moreover, our data suggest that amyloid beta and tau pathology actually lie downstream of mitochondrial dysfunction in the progression of Alzheimer’s disease, which opens up a new therapeutic angle.”
The researchers plan to work on further describing the metabolic dysfunction that occurs before symptoms of Alzheimer’s appear.