Subcutaneous injections of Eisai and Biogen’s Leqembi led to numerically greater amyloid removal than the intravenous version of the Alzheimer’s disease therapy, though risks of brain swelling and bleeding remained.
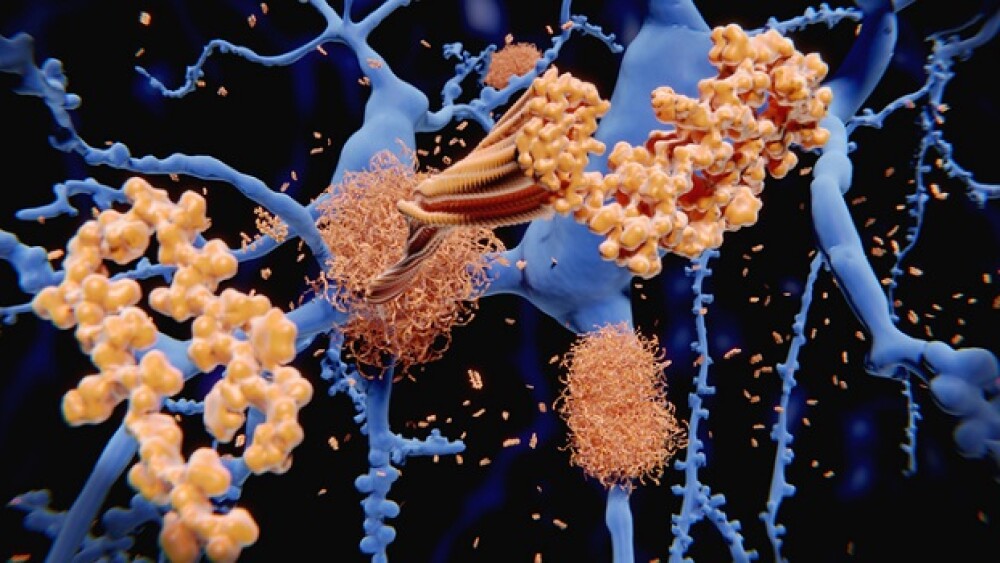
Pictured: Amyloid plaques disrupting neuronal networks/iStock, selvanegra
Eisai and Biogen on Wednesday unveiled new data from the open-label extension phase of the Clarity AD study, showing that the subcutaneous formulation of its Alzheimer’s disease therapy Leqembi (lecanemab) is also effective at clearing amyloid plaques in the brain.
However, safety concerns remain including MRI signals that might indicate brain swelling and bleeding. The pharma partners presented the results at the 2023 Clinical Trials on Alzheimer’s Disease (CTAD) conference.
Compared with biweekly intravenous doses of Leqembi, weekly subcutaneous injections achieved an approximately 14% higher removal of amyloid plaques in the brain after six months of treatment. The under-the-skin injection also resulted in a stronger pharmacokinetic profile than the approved infusions.
In terms of safety, the study detected a slightly higher rate of amyloid-related imaging abnormalities (ARIA) in the subcutaneous Leqembi group, though the differences in frequencies were not statistically significant.
ARIA refers to the broad category of abnormal MRI findings in patients taking amyloid-modifying treatments for Alzheimer’s disease (AD). In its approved form, Leqembi’s label carries a boxed warning for ARIA, which is typically asymptomatic but can lead to “serious and life-threatening events” in rare cases.
In Clarity AD’s open-label extension phase, ARIA signals indicative of cerebral edema—or brain swelling—were found in 16.7% of patients given subcutaneous Leqembi compared to 12.6% in the intravenous formulation. ARIA suggestive of brain bleeding were detected in 22.2% and 17.3% of the subcutaneous and intravenous group, respectively.
“We were hoping, based on the Phase II and Phase III data, that the ARIA rates would be less,” Michael Irizarry, Eisai’s deputy chief clinical officer and head of clinical neurology research, told Endpoints News.
Leqembi is a monoclonal antibody that targets and binds to toxic amyloid-beta plaques, neutralizing them and promoting their clearance from the brain. It first won the FDA’s accelerated approval in January 2023, which was later converted to traditional approval in July.
With these data from the open-label extension of Clarity AD, Biogen and Eisai will work toward another regulatory approval for Leqembi and expect to file a Biologics License Application for the subcutaneous formulation by March 31, 2024.
Separately, the partners also presented tau protein data for Leqembi, showing in a post-hoc analysis that the therapeutic antibody could induce cognitive improvements in 60% of patients with low tau levels— indicative of earlier-stage Alzheimer’s—after 18 months of treatment. Only 28% of placebo comparators achieved such improvement.
Tristan Manalac is an independent science writer based in Metro Manila, Philippines. He can be reached at tristan@tristanmanalac.com or tristan.manalac@biospace.com.