FibroGen, Inc. (NASDAQ:FGEN), today announced results from the pooled analyses of data from six global pivotal Phase 3 trials investigating roxadustat, a first-in-class, orally-administered inhibitor of hypoxia-inducible-factor (HIF) prolyl hydroxylase activity.
WASHINGTON, Nov. 08, 2019 (GLOBE NEWSWIRE) -- FibroGen, Inc., (NASDAQ:FGEN), today announced results from the pooled analyses of data from six global pivotal Phase 3 trials investigating roxadustat, a first-in-class, orally-administered inhibitor of hypoxia-inducible-factor (HIF) prolyl hydroxylase activity. The pooled analyses assessed the safety and efficacy of roxadustat as a treatment for anemia in chronic kidney disease (CKD) compared to placebo in Non-Dialysis-Dependent (NDD) patients and to standard of care epoetin alfa in Dialysis-Dependent (DD) patients, including the clinically important Incident Dialysis (ID) patient subgroup. These Phase 3 trials conducted by FibroGen and collaboration partners AstraZeneca and Astellas Pharma, Inc., enrolled over 8,000 CKD patients from more than 50 countries.
“The pooled safety analyses assessing roxadustat as a treatment for anemia in chronic kidney disease demonstrate a cardiovascular safety profile comparable with placebo in patients not on dialysis, and comparable or in some cases better than that of epoetin alfa in patients on dialysis,” said Robert Provenzano, MD, Associate Professor of Medicine, Wayne State University, Detroit, Michigan, U.S. and a primary investigator on the global Phase 3 program. “It is exciting to see this application of the groundbreaking science on oxygen sensing and adaptation to hypoxia recently awarded the 2019 Nobel Prize in Physiology or Medicine, and championed by FibroGen’s late founder and CEO, Tom Neff, who sadly passed away earlier this year. These positive safety results, coupled with roxadustat’s well-defined efficacy in CKD patients, and its oral formulation, support the potential for roxadustat to become an important new treatment option for patients with anemia associated with CKD.”
These late-breaking data were featured in the High-Impact Clinical Trials oral abstract session on Friday, November 8, at the American Society of Nephrology Kidney Week 2019 in Washington, D.C. (Presentation FR-OR131)
Pooled Efficacy Results
Individually, all six Phase 3 trials included in these pooled analyses (OLYMPUS, ANDES, ALPS, HIMALAYAS, SIERRAS, and ROCKIES) achieved the primary efficacy endpoint of mean hemoglobin (Hb) change from baseline compared to placebo in patients not on dialysis and to epoetin alfa in patients on dialysis.
In the pooled analysis of Non-Dialysis Dependent (NDD) patients (n=4277):
- Roxadustat was statistically superior to placebo, demonstrating an improvement of 1.85 g/dL in patients’ Hb levels from baseline to the average over 28-52 weeks compared to 0.13 g/dL among patients in the placebo arm, for an overall treatment difference of 1.72 g/dL (p<0.001).
- The rate of rescue therapy required in the first year of treatment among patients treated with roxadustat (8.9%) was less than one third of the rate of the placebo arm (31.1%) p<0.0001; HR=0.19 (95% CI: 0.16, 0.23).
- The rate of red blood cell (RBC) transfusions required in the first year of treatment was also lower with roxadustat (5.2%) than placebo (15.4%) p<0.0001; HR=0.26 (95% CI: 0.21, 0.32).
In the pooled analysis of Dialysis Dependent (DD) patients (n=3880):
- Roxadustat was statistically superior to epoetin alfa, demonstrating an improvement of 1.22 g/dL in patients’ Hb levels from baseline to the average over 28-52 weeks compared to 0.99 g/dL, for an overall treatment difference of 0.23 g/dL (p<0.0001).
- Roxadustat was superior to epoetin alfa across patients regardless of inflammation status, categorized by the baseline CRP levels (CRP > 4.9 mg/L), demonstrating an improvement of 1.29 g/dL and 1.27 g/dL in Hb levels from baseline in patients with and without inflammation, respectively, compared to 0.96 g/dL and 1.05 g/dL with epoetin alfa.
- The rate of RBC transfusions required in the first year of treatment was also lower with roxadustat (9.5%) than with epoetin alfa (12.8%) in DD patients (p=0.046). HR=0.82 (95% CI: 0.679, 0.997).
Across the NDD and DD patient populations, roxadustat was effective in raising Hb levels regardless of whether patients were iron-replete (i.e., shown to have sufficient stores of iron in their body, TSAT% ≥20% and Ferritin ≥100 ng/mL) at baseline. NDD patients experienced a mean change of 1.94 g/dL from baseline with roxadustat in both iron-replete and non-replete subpopulations, compared to 0.13 g/dL in iron-replete and 0.33 g/dL in non-replete patients receiving placebo.
Pooled Safety Results
Across these pooled safety analyses, the studies evaluated several different patient populations, including:
- Non-Dialysis Dependent (NDD) patients;
- Dialysis Dependent (DD) patients; and
-- Incident Dialysis (ID) patients, who are patients who recently initiated dialysis (within 4 months). This ID subpopulation is the appropriate setting for comparison of roxadustat versus epoetin alfa, as this period of initial dialysis treatment is associated with substantially increased levels of safety events and patient mortality; whereas the stable DD patients have survived this period and thus are responsive to stable doses of erythropoiesis stimulating agents (ESA) such as epoetin alfa.
Cardiovascular (CV) endpoints were defined as:
- Time to first Major Adverse Cardiovascular Event (MACE): a composite endpoint of all-cause mortality, myocardial infarction, stroke;
- Time to first MACE+, a composite endpoint which includes MACE plus unstable angina and heart failure requiring hospitalization; and
- Time to all-cause mortality
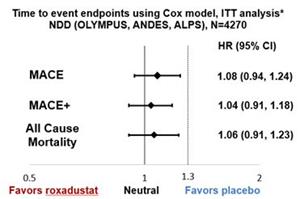
-- In the Non-Dialysis Dependent (NDD) patient population:
- Risks of MACE, MACE+, and all-cause mortality in roxadustat patients were comparable to placebo in the ITT analyses based on a reference non-inferiority margin of 1.3.
-- In a post hoc subgroup analysis of 2,438 non-dialysis patients with baseline eGFR≥15,
- The one-year decline in eGFR in roxadustat treated patients (-2.8) was significantly less than that in placebo treated patients (-4.4), with a treatment difference of 1.6 mL/min/1.73m2 (p<0.0001).
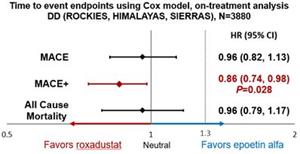
-- In the Dialysis Dependent (DD) patient population:
- Risks of MACE and all-cause mortality in roxadustat patients were not increased compared to those for patients receiving epoetin alfa based on a reference non-inferiority margin of 1.3.
- Risk of MACE+ was 14% lower in roxadustat-treated patients than in those receiving epoetin alfa.
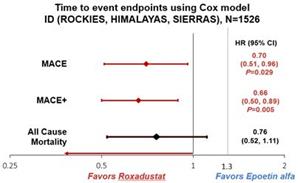
-- The Incident Dialysis (ID) patient sub-group of the Dialysis Dependent (DD) patient population:
- Risk of MACE was 30% lower in roxadustat patients than in epoetin alfa patients, and risk of MACE+ was 34% lower.
- Roxadustat-treated patients’ risk showed a trend towards lower all-cause mortality relative to epoetin alfa-treated patients.
“The positive efficacy and cardiovascular safety results from these pooled analyses, in a population with a broad range in both CKD and anemia severity in over 8,000 patients across six Phase 3 global trials, reaffirm the potential of roxadustat to improve treatment for anemia in CKD patients.” said K. Peony Yu, MD, Chief Medical Officer, FibroGen. “There has not been much progress in treatment approaches for anemia in over 30 years, and more effective, safe, and convenient treatment options for patients are long overdue. We are privileged to be advancing this effort with roxadustat and plan to file the NDA in the U.S. by the end of this quarter for both dialysis and non-dialysis patients with our partner AstraZeneca and the MAA in Europe by the end of first quarter 2020 with our partner Astellas, followed by submissions to other regulatory authorities.”
About Anemia Associated with CKD
Anemia can be a serious medical condition in which patients have insufficient red blood cells and low levels of hemoglobin, a protein in red blood cells that carries oxygen to cells throughout the body. Anemia in CKD is associated with increased risk of hospitalization, cardiovascular complications and death, also frequently causing significant fatigue, cognitive dysfunction and reduced quality of life. Severe anemia is common in patients with CKD, cancer, myelodysplastic syndromes (MDS), inflammatory diseases, and other serious illnesses.
Anemia is particularly prevalent in patients with CKD. The prevalence of CKD in the adult population is estimated at 10-12% globally and is generally a progressive disease characterized by gradual loss of kidney function that may eventually lead to kidney failure, or end stage renal disease, requiring dialysis or kidney transplant to survive. Blood transfusion is used for treating life-threatening severe anemia. However, blood transfusions reduce the patient’s opportunity for kidney transplant, increase risk of infections and the risk of complications such as heart failure and allergic reactions.
According to the United States Renal Data System (USRDS), over 14% of the U.S. adult population is affected by CKD, and a majority of dialysis-eligible CKD patients are currently on dialysis. It is estimated that approximately 509,000 patients are receiving dialysis in the U.S. as of 2016.
About Roxadustat
Roxadustat (FG-4592) is a first-in-class, orally administered small molecule HIF-PH inhibitor that promotes erythropoiesis through increasing endogenous production of erythropoietin, improving iron regulation, and overcoming the negative impact of inflammation on hemoglobin syntheses and red blood cell production by downregulating hepcidin. Administration of roxadustat has been shown to induce coordinated erythropoiesis, increasing red blood cell count while maintaining plasma erythropoietin levels within or near normal physiologic range in multiple subpopulations of chronic kidney disease (CKD) patients, including in the presence of inflammation and without a need for supplemental intravenous iron. Roxadustat is currently approved in China for the treatment of anemia in CKD patients on dialysis and patients not on dialysis and approved in Japan for the treatment of anemia in CKD patients on dialysis. Roxadustat is in Phase 3 clinical development in the U.S. and Europe and in Phase 2/3 development in China for anemia associated with myelodysplastic syndromes (MDS), and in a Phase 2 U.S. trial for treatment of chemotherapy-induced anemia.
Astellas and FibroGen are collaborating on the development and commercialization of roxadustat for the treatment of anemia in territories including Japan, Europe, the Commonwealth of Independent States, the Middle East, and South Africa. AstraZeneca and FibroGen are collaborating on the development and commercialization of roxadustat for the treatment of anemia in the U.S., China, and other markets in the Americas and in Australia/New Zealand as well as Southeast Asia.
About FibroGen
FibroGen, Inc., headquartered in San Francisco, California, with subsidiary offices in Beijing and Shanghai, People’s Republic of China, is a leading biopharmaceutical company discovering and developing a pipeline of first-in-class therapeutics. The company applies its pioneering expertise in hypoxia-inducible factor (HIF) and connective tissue growth factor (CTGF) biology, and clinical development to advance innovative medicines for the treatment of anemia, fibrotic disease, and cancer. Roxadustat, the company’s most advanced product candidate, is an oral small molecule inhibitor of HIF prolyl hydroxylase (HIF-PH) activity, completing worldwide Phase 3 clinical development for the treatment of anemia in chronic kidney disease (CKD), is approved by the National Medical Products Administration (NMPA) in China for CKD patients on dialysis and not on dialysis and by the Ministry of Health, Labour and Welfare in Japan for CKD patients on dialysis. Roxadustat is in Phase 3 clinical development in the U.S. and Europe and in Phase 2/3 development in China for anemia associated with myelodysplastic syndromes (MDS), and in a Phase 2 U.S. trial for treatment of chemotherapy-induced anemia. Pamrevlumab, an anti-CTGF human monoclonal antibody, is in Phase 3 clinical development for the treatment of idiopathic pulmonary fibrosis (IPF) and pancreatic cancer, and is currently in a Phase 2 trial for Duchenne muscular dystrophy (DMD). FibroGen is also developing a biosynthetic cornea in China. For more information, please visit www.fibrogen.com.
Forward-Looking Statements
This release contains forward-looking statements regarding our strategy, future plans and prospects, including statements regarding the development of roxadustat, our interpretation of the pooled safety analyses and other analyses of the global Phase 3 program for roxadustat, , the potential for and timing of an NDA submission to the FDA and an MAA submission to the EMA for potential marketing approval for roxadustat, the potential safety and efficacy profile of our product candidates, aspects of roxadustat that could affect its commercial prospects, and our clinical, regulatory plans, and those of our partners. These forward-looking statements include, but are not limited to, statements about our plans, objectives, representations and contentions and are not historical facts and typically are identified by use of terms such as “may,” “will”, “should,” “on track,” “could,” “expect,” “plan,” “anticipate,” “believe,” “estimate,” “predict,” “potential,” “continue” and similar words, although some forward-looking statements are expressed differently. Our actual results may differ materially from those indicated in these forward-looking statements due to risks and uncertainties related to the continued progress and timing of our various programs, including the enrollment and results from ongoing and potential future clinical trials, and other matters that are described in our Annual Report on Form 10-K for the fiscal year ended December 31, 2018, and our Quarterly Report on Form 10-Q for the fiscal quarter ended June 30, 2019 filed with the Securities and Exchange Commission (SEC), including the risk factors set forth therein. Investors are cautioned not to place undue reliance on these forward-looking statements, which speak only as of the date of this release, and we undertake no obligation to update any forward-looking statement in this press release, except as required by law.
Contact:
FibroGen, Inc.
Media Inquiries:
Sara Iacovino
1.703.474.4452
sara.iacovino@gcihealth.com
Investors:
Michael Tung, M.D.
Investor Relations
1.415.978.1433
ir@fibrogen.com
Photos accompanying this announcement are available at
https://www.globenewswire.com/NewsRoom/AttachmentNg/42940076-9101-4178-8cee-ac4a9f974ecb
https://www.globenewswire.com/NewsRoom/AttachmentNg/11e33b31-2f3d-4905-8960-a5f165353fae
https://www.globenewswire.com/NewsRoom/AttachmentNg/89c53228-2d1d-43e1-9433-52ee642a4ff9
IMAGE 1
Time to event endpoints using Cox model, ITT analysis* NDD (OLYMPUS, ANDES, ALPS), N=4270*ITT analysis agreed with the FDA
IMAGE 2
Time to event endpoints using Cox model, on-treatment analysis DD (ROCKIES, HIMALAYAS, SIERRAS), N=3880
IMAGE 3