In the study published October 7th in Science Translational Medicine, Dr. Weiss et al shared that immunocytokines delivered systemically were effective in mice models and a pilot human trial.
Glioblastoma is an aggressive and usually terminal form of brain cancer that carries a median survival rate of only 15-18 months. That rate is twice what it was twenty years ago, and researchers are still looking to extend it even further. Immunocytokines showed promise in a recent study led by Tobias Weiss, a senior physician and researcher at the University Hospital Zurich (UHZ).
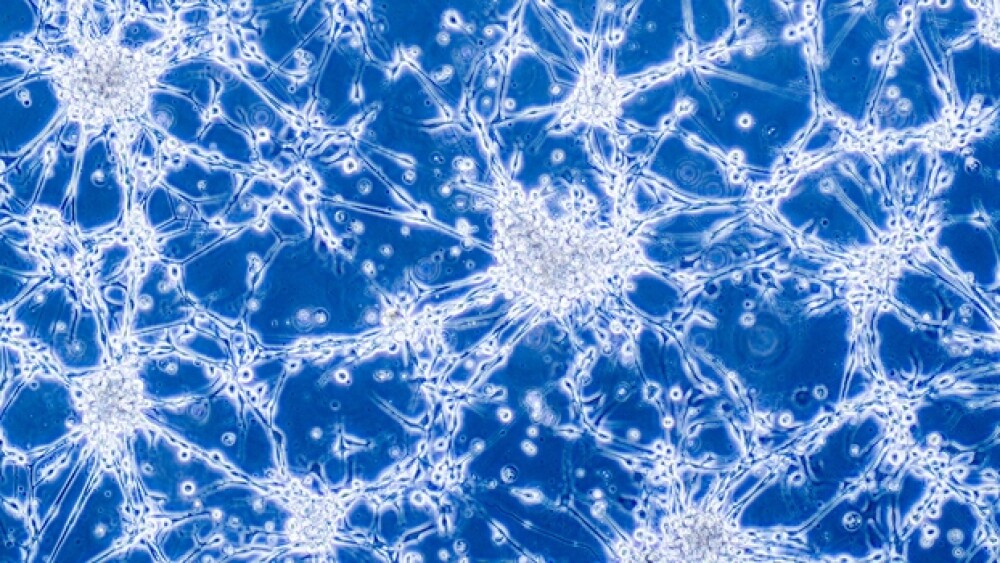
The lethality of glioblastoma is partly due to the strong immunosuppressive tumor environment of the glioma cell, which prevents the immune system from fighting back.
Despite recent successes with extracranial immunotherapies, these victories have not translated to invasive cancers such as glioblastomas, so Weiss and team turned their attention to immunocytokines, which are antibody-cytokine-fused proteins.
One hypothesis is that these proinflammatory cytokines may trigger a strong antitumor immunity, subsequently converting the immunological “cold” microenvironment normally found in glioblastoma into an immunologically “hot” tumor microenvironment.
In the study published October 7th in Science Translational Medicine, Dr. Weiss et al shared that immunocytokines delivered systemically were effective in mice models and a pilot human trial.
The team created three immunocytokines based on the L19 antibody, which is specific to the extracellular matrix of the glioblastoma tumor. The immunocytokines, L19-mTNF and L19-mIL12, were then intravenously injected fully immunocompetent mice pretreated with orthotopic GL-261 gliomas. L19 alone was used as a control.
The results indicated a stable safety profile, while the treatment was effective in decreasing regional blood perfusion within the tumor and contributed to the increase of tumor necrosis.
Because glioblastoma tumors have shown such resistance to immunotherapy in the past, that the scientists issued a second challenge to test the therapy’s staying power.
“After 180 days from the first tumor cell implantation, we implanted a second set of tumor cells into the contralateral hemisphere from the hemisphere that received the first implanted tumor cells. In the absence of any further therapeutic intervention, all long-term surviving mice were protected from tumor growth and survived,” Weiss et al said in the paper.
Currently, the typical course of treatment is a three-pronged attack with surgery to remove the tumor, radiation to remove the remaining cells and chemotherapy with drugs such as Temozolomide (Temodar), which is considered the gold standard for glioblastoma.
There are additional cutting-edge approaches being studied to meet the critical unmet need in effective glioblastoma treatment. These include gene therapy, which attempts to overcome barriers such as chemotherapy resistance by downregulating resistance genes, and a new method of radiation therapy that works by targeting a critical metabolic pathway to disrupt the tumor’s ability to repair itself.
October 24 is National Brain Cancer Awareness Day in Canada. In the U.S, all are encouraged to “Go Gray” in May.