Peter Jones, a professor of pharmacology at the University of Nevada in Reno, has been researching the disease for years and may have helped to unlock one of the first treatments for the disease.
“Everything about FHSD is weird.”
Facioscapulohumeral muscular dystrophy (FHMD) is one of the most common forms of the disease, but many people who have it are unaware that this type of MD is the root cause of their progressive weakness. Peter Jones, a professor of pharmacology at the University of Nevada in Reno, has been researching the disease for years and may have helped to unlock one of the first treatments for the disease.
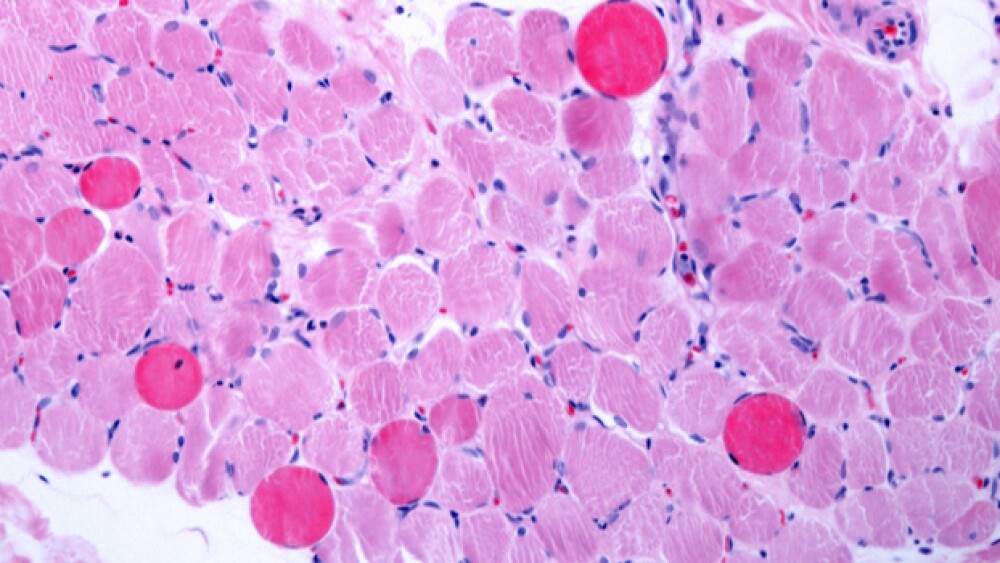
FSHD is an adult-onset form of MD that normally hits patients in their early 20s and 30s. FHMD is the most common form of muscular dystrophy, affecting about 40,000 people across the United States. The disease is caused by the mis-expression of the DUX4 gene in skeletal muscle. The presence of DUX4 proteins become toxic to muscle tissue and causes degeneration that results in significant physical limitations, including an inability to smile and difficulty using arms for activities. Many FSHD patients become dependent upon the use of a wheelchair for daily mobility.
Research led by Jones has shown that strategies to control the expression of DUX4 expression may have potential applications in the treatment of FSHD. The role of DUX4 in FSHD has only become understood in the last decade. In adults, the DUX4 gene is normally “off,” Jones said, but in FSHD patients, a mutation has caused the gene to “turn on.” But, it takes a significant amount of time for that mutation to really begin to manifest in the form of progressive weakness of the muscle. Jones described it as a weight hanging by a rope from the ceiling. The drag of that weight isn’t as noticeable until the strands of the rope begin to separate. Once it separates, that’s when the weight falls and, in the case of FSHD, the weakness in the muscles begin to present.
“There’s a huge variability to the way it’s expressed in the body. It’s almost like each patients is different but the fundamental mechanism is the same,” Jones told BioSpace in an exclusive interview.
Over the course of FSHD research, Jones (and others who work on the disease) learned that DUX4 doesn’t have to be shut off to halt the disease, but could be “dialed down” in order to demonstrate a therapeutic benefit.
“Any reduction of DUX4 level will most likely have therapeutic benefit,” Jones said. “You don’t really have to turn it off, just dial it back. If there’s a drug that turns it back by 40%, you could see tremendous benefit.”
With that understanding, some pharma companies are aiming their research at DUX4, including Fulcrum Therapeutics, for which Jones serves as a scientific advisor. In October, Cambridge, Mass.-based Fulcrum announced preliminary results of its Phase I FSHD treatment losmapimod, a selective p38α/β mitogen activated protein kinase inhibitor. The drug has now moved into Phase II and Jones said, to his knowledge, that Fulcrum is now the only company that has a treatment for FSHD in the clinic. One month prior to Fulcrum’s October announcement and Jones could not have made that claim. However, in September, Acceleron Pharma killed its mid-stage FSHD program following its failure to hit secondary endpoints. Instead of targeting DUX4, Acceleron’s ACE-083 attempted to outpace the disease by increasing muscle strength and function in specific target muscles.
“What happened with Acceleron was a great example of not addressing the underlying issue of the disease. It was like having a hole in the boat and trying to bail it out faster than water comes in,” Jones said.
Fulcrum is going after the root cause of the disease, he added. Now the question awaiting the company, and the FSHD world is whether or not the approach will achieve the desired benefit. Fulcrum doesn’t anticipate data until the fall of this year.
“I’m hopeful that it works, he said.
While Fulcrum moved forward in the clinic, other companies are taking aim at the disease but remain in the preclinical phase. One example is San Diego-based Genea Biocells. In 2018 the company picked up Orphan Drug designation from the U.S. Food and Drug Administration for GBC0905, a small molecule that suppresses DUX4 function.