A protein called ACE2 is intimately involved in how SARS-CoV-2, the virus that causes COVID-19, infects the body.
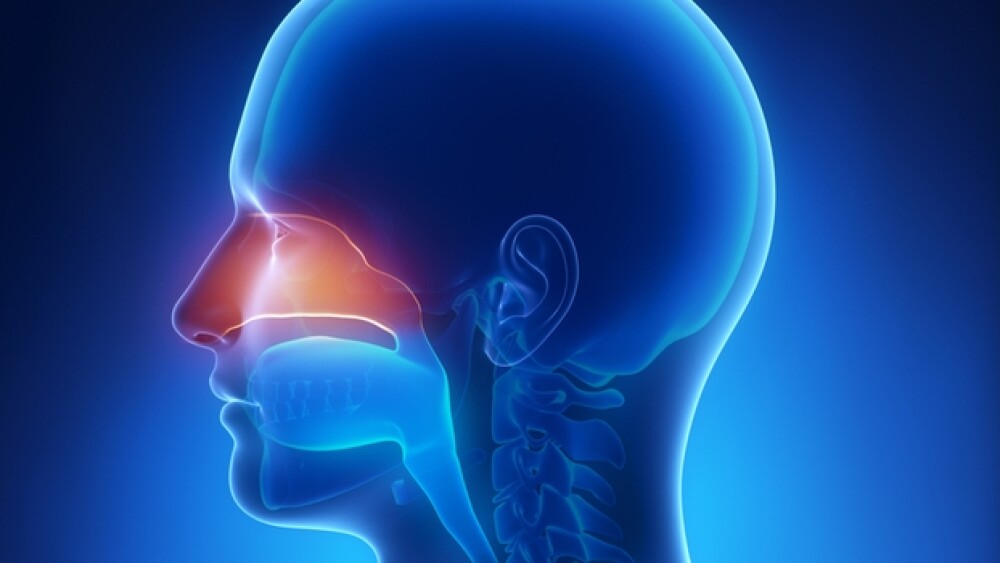
A protein called ACE2 is intimately involved in how SARS-CoV-2, the virus that causes COVID-19, infects the body. The protein is found on nasal membrane cells, which is typically where the virus enters the body. The ACE2 protein is found throughout the body in various concentrations, but it is in the lungs, heart and kidneys, as well as lining of the blood vessels. There is now research suggesting that one reason children may be less likely to be infected is because of their relatively fewer ACE2 proteins.
A March 30, 2020 article in The New England Journal of Medicine noted that the renin-angiotensin-aldosterone system (RAAS) is a cascade of vasoactive peptides that are involved in a number of key processes in humans. ACE2 interfaces with the RAAS system, with the ACE2 enzyme countering RAAS activation but also acting as a receptor for both SARS-CoV-1 and SARS-CoV-2 (the first causing SARS, the second causing COVID-19).
The most recent research was published in the medical journal JAMA (the Journal of the American Medical Association). It notes, “Children account for less than 2% of identified cases of coronavirus disease 2019 (COVID-19). It is hypothesized that the lower risk among children is due to differential expression of angiotensin-converting enzyme 2 (ACE2), the receptor that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) uses for host entry.”
Their research studied the ACE2 gene expression in the nasal epithelium of children and adults. In 305 people aged 4 to 60 years, with about an even mix of males and females, they found ACE2 gene expression was lowest in younger children and increased with age. In the youngest group it was 2.40 counts per million, in older children it was 2.77 counts/million, for young adults it was 3.02 counts/million and in adults, 3.09 counts/million. They also noted that the cohort was originally recruited to study biomarkers for asthma, so as a result, 49.8% of the study group had been diagnosed with asthma.
The age breakdown was into four groups: less than 10, 10 to 17, 18 to 24, and older than 24. There was no difference in the amount of ACE2 RNA by gender or with patients with or without asthma. But the amount of ACE2 RNA did increase with age.
The study did not measure directly the protein responsible for viral attachment, but instead measured the RNA that directs the production of the protein in the body in particular cells—membrane cells in the nose. The Forbes article notes, “Usually but not always, the amount of RNA in cells determines the amount of the corresponding protein. The authors assume that is the case, and their conclusion depends on that assumption.”
The Forbes article, written by William A. Haseltine, a former professor at Harvard Medical School, where he founded two academic research departments, the Division of Biochemical Pharmacology and the Division of Human Retrovirology, noted that, “The differences are relatively small and the error bars large. The average relative amount of RNA ranges from 2.4 for those less than 10 to 3.09 for those 25 and older. However, when the probable range is included, the results from the three older groups overlaps, as do the results from the three younger groups.”
So is it possible to conclude that the reason children are less likely to get COVID-19 because they have fewer ACE2 receptors in their nose? And for that matter, is that why the disease is more likely to affect an older population, especially the elderly?
The answer is maybe, but it’s not definite. One problem is nobody yet knows just how many receptors are needed for the SARS-CoV-2 virus to successfully infect people, or, for that matter, what kind of viral load is needed for it to happen (and for that load to overwhelm the individual’s immune system).
Although less common, young children can be infected.
Haseltine writes, “Additionally, we do not know the efficiency of the conversion of RNA to the stable ACE2 protein that serves as a receptor. Also unknown is whether or not there are age related biological and behavioral factors other than ACE2 which determine susceptibility to infection.”
It was only relatively recently that a Kawaski-like disease in young children was associated with COVID-19 patients. COVID-19 is quite rare in younger children, 1.7% in the U.S., 1% in the Netherlands, 2.0% in the U.K.
The syndrome associated with the children looks like Kawaski disease and toxic shock syndrome. The U.S. Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) called it multisystem inflammatory syndrome in children (MIS-C), but it is also called “pediatric multisystem inflammatory syndrome” and “pediatric hyperinflammatory syndrome.”
Kawasaki disease is an inflammatory illness that primarily affects children age 5 and younger. Its causes are unknown. Toxic shock syndrome comes from bacterial infection and results in severe inflammation and is deadlier than Kawasaki disease. Both conditions share symptoms with MIS-C, including fever, red eyes, skin rash and body pains. But MIS-C is classified as a distinct syndrome.
MIS-C is very rare and most patients have responded well to treatment and fully recovered.