Recent research suggests that it may be possible to categorize GBM into different subtypes based on the underlying biological mechanisms driving tumor development and growth.
Glioblastoma (GBM) is a highly lethal type of brain cancer that is notoriously difficult to treat. While the 5-year survival rate for all types of brain cancer is 33%, GBM has a 5-year survival rate of only 5%. Despite its historically poor prognosis, however, GBM patients may have new reasons to be hopeful based on recent advances in both research and medical technologies.
GBM heterogeneity poses challenges for long-term treatment
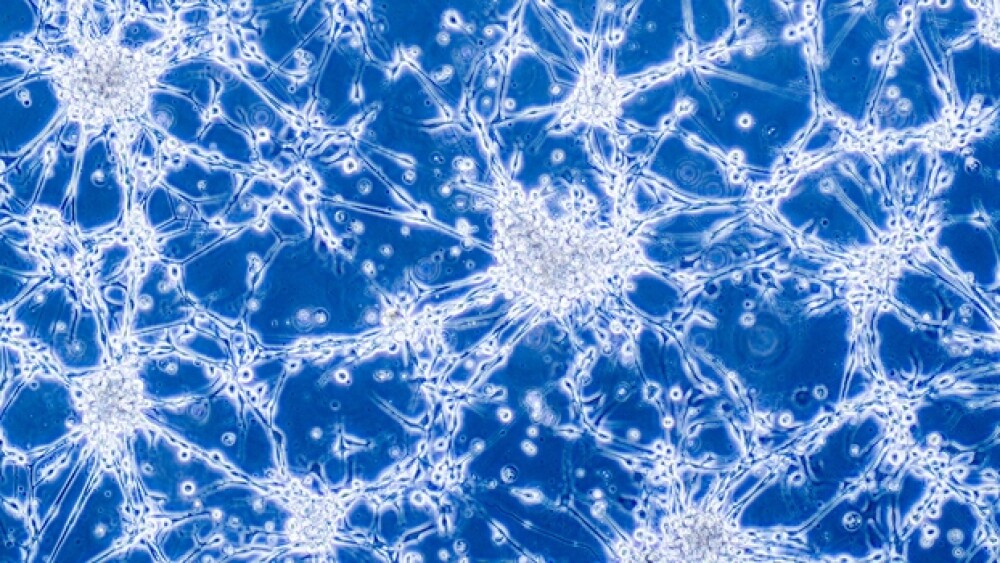
GBM is a highly complex and heterogeneous disease that can involve a large variety of genetic, molecular and cellular mechanisms. For this reason, treatment efficacy can vary significantly across patients and it can be difficult for doctors to predict which treatment options will be most effective for a given patient.
Recent research suggests that it may be possible to categorize GBM into different subtypes based on the underlying biological mechanisms driving tumor development and growth. Identification of different GBM subtypes may help doctors identify the most appropriate treatment options for each patient.
Identification of mitochondrial GBM subtype offers potential new treatment avenues
In a recent study published in Nature Cancer, scientists at Columbia University’s Vagelos College of Physicians and Surgeons and Herbert Irving Comprehensive Cancer Center grouped GBM into four different categories based on the tumors’ core biological features.
This method of classification differs from most previous attempts at classification, which typically try to define tumors based on their genetic characteristics. The scientists argue that classifying tumors by their biological characteristics rather than underlying genetic composition may provide better insight into what treatments will work best for patients.
One of the GBM subtypes the scientists identified is a mitochondrial subtype. Mitochondria are specialized structures inside cells that act as a sort of ‘battery’ to fuel biochemical processes. In the mitochondrial GBM subtype, mitochondria are overactive.
The scientists discovered that mitochondria-inhibiting drugs can inhibit tumor growth in both laboratory-grown cells and in mice. These findings are promising given that they open new potential avenues for GBM treatment in humans with mitochondria-inhibiting drugs, some of which are already undergoing testing in clinical trials.
Combined radiation and small molecule therapy may provide new treatment option for newly diagnosed GBM patients with specific genetic characteristics
In another attempt to provide more targeted therapies to specific subsets of GBM patients, Denovo Biopharma began Phase III trials in January examining the small molecule enzastaurin (DB102) in combination with temozolomide (Temodar) and radiotherapy.
In the trials, scientists use a novel biomarker, Denovo Genomic Marker 1 (DGM1), to identify a subset of GBM patients who are most likely to benefit from enzastaurin therapy combined with temozolomide and radiotherapy.
The study is the second Phase III trial to evaluate enzastaurin in patients with cancer - the first study was conducted in patients with diffuse large B-cell lymphoma (DLBCL). The DLBCL trials also used DGM1 to identify the patients who would likely receive the most benefit of enzastaurin in combination regimens.
Based on earlier studies showing a high correlation between DGM1 and response to enzastaurin, enzastaurin combination regimens have the potential to improve survival odds in GBM patients with DGM1.
New drug-device combination treatment for GBM may ‘turn GBM into a manageable disease’
Another promising GBM therapy on the horizon comes from a collaborative effort by the Ivy Brain Tumor Center at the Barrow Neurological Institute in Phoenix, SonALAsense, a company with headquarters in Berkeley, California, and InsightTec, a company headquartered in Haifa, Israel. The therapy, called sonodynamic therapy (SDT), is a non-invasive GBM treatment that combines SonALAsense’s proprietary formulation of aminolevulinic acid (ALA) with InSightec’s incisionless MR-guided focused ultrasound technology.
In animal studies, the combined ALA-SDT treatment was found to quickly kill tumor cells while simultaneously triggering apoptosis (programmed cell death). Now, the therapy will undergo human trials.
In humans, ALA will be injected intravenously, after which it can be absorbed by GBM cells. GBM cells have a unique metabolic composition (which is different from normal brain cells) that causes them to absorb large amounts of ALA. Once absorbed, GBM cells convert ALA to a fluorescent molecule called protoporphyrin.
“Protoporphyrin is key, because protoporphyrin can do two things,” Stuart Marcus, M.D., Ph.D., told BioSpace. “If you have a lot of protoporphyrin, you can activate it with light and it can release that energy as fluorescence, and you can use it as a tumor marker. Or, if you use a higher energy of light, you can use photodynamic therapy. If this is done in a tumor cell, it will punch holes in the membrane, and the cell will die. It can also knock holes in the mitochondria membrane which will then release cytochrome c and cause apoptosis.”
Marcus is SonALAsense’s founder, CEO and CMO.
While ALA-SDT technology is a new treatment for GBM, similar treatments have been used to treat other types of cancer, like skin cancer, and have proven to be highly effective. Unlike ALA-SDT, which uses sound to activate protoporphyrin, therapies for skin cancer have used photodynamic therapy (PDT), which uses light to activate protoporphyrin. Marcus led the clinical development and FDA approval of the ALA-PDT system.
While PDT is a feasible option for skin cancer, it is less feasible for brain cancer. To activate protoporphyrin in the brain using light, invasive optical probes are needed, requiring complex and potentially dangerous brain surgery. By using sound waves, SDT can activate protoporphyrin without the need for invasive surgical procedures.
Based on the success of ALA-PDT in skin cancers, Marcus and the SonALAsense team have high hopes for ALA-SDT therapy for GBM.
“It will be the first non-invasive, tissue-specific treatment that has the potential to turn glioblastoma into a manageable disease and glioblastoma patients into cancer survivors,” Marcus said.