UCLA Jonsson Comprehensive Cancer Center researchers and their colleagues announced on May 1 that they have discovered a drug that may help improve the overall survival rate in glioblastoma patients.
UCLA Jonsson Comprehensive Cancer Center researchers and their colleagues announced on May 1 that they have discovered a drug that may help improve the overall survival rate in glioblastoma patients.
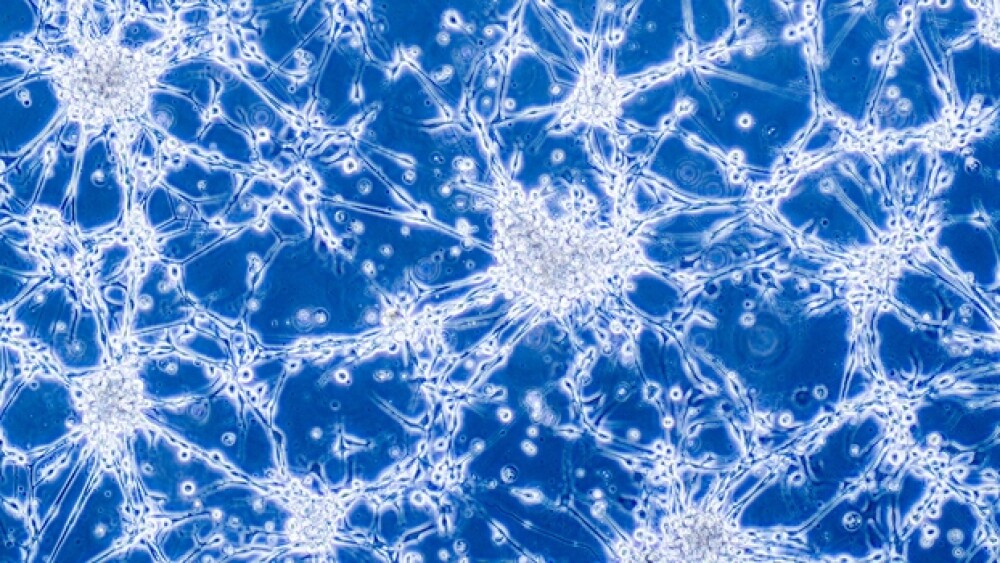
Their findings, which were published in Proceedings of the National Academy of Sciences, looked at trifluoperazine and how it impacted mice with glioblastoma, a difficult-to-treat brain tumor. The drug, which was once commonly used to treat schizophrenia, appeared to target glioblastoma cells in the body. In addition, it appeared to help overcome the resistance to treatment common to this form of cancer.
Radiation is one of the most effective form of treatments for patients with glioblastoma. However, the tumor cells often become resistant to radiation treatment because the radiation itself can induce “phenotype conversion.” This process turns non-tumor stem cells into tumor-producing cells, causing the cancer to reoccur. UCLA researchers have been looking into new ways to prevent glioblastoma tumor cells from becoming resistant to radiation treatment by adding drugs to patients’ treatment regimen.
“While radiotherapy is one of the few treatments that prolong survival in glioblastoma patients, radiation alone does very little in treating the disease in our models because we are dealing with highly aggressive tumors,” said the study’s senior author, Dr. Frank Pajonk, a professor of radiation oncology at the David Geffen School of Medicine at UCLA and a member of the Jonsson Cancer Center. “The drug trifluoperazine by itself does not do much either, but we found when you combine them, they become highly efficient. Importantly, the drug does not sensitize cells to radiation but rather prevents the occurrence of resistant glioma stem cells.”
The researchers and their colleagues looked at more than 83,000 compounds through shared resources at UCLA to determine if there are any existing drugs that could interfere with radiation-induced phenotype conversion. They identified almost 300 compounds, including trifluoperazine, that could potentially block phenotype conversion and improve the efficacy of radiation therapy.
Trifluoperazine was ultimately tested in mice with patient-derived orthotopic tumors. The team found that, in combination with radiation, trifluoperazine delayed the growth of tumors and prolonged the survival of the mice. This summer, the team intends to begin a clinical trial for people with recurrent glioblastoma.
“Many preclinical glioblastoma studies report fairly small increases in overall survival in mice, and that rarely translates into benefits for patients,” Pajonk continued. “But here we see pretty drastic effects in improved overall survival, and I find that very encouraging. It gives us hope that this is all going to translate into a benefit for people.”
In April, AIVITA Biomedical, Inc. revealed updated survival data from a year-end analysis of its ongoing Phase II clinical trial of AV-GBM-1 in patients with newly diagnosed glioblastoma. The overall survival rate at both 12 and 15 months was 76% in AV-GBM-1-treated patients, compared to an overall survival rate of 61% at 12 months and 48% at 15 months in control patients.
“Although treatment and monitoring of patients is ongoing, we are very encouraged by these interim results,” said Dr. Robert O. Dillman, AIVITA Chief Medical Officer. “We completed accrual to the trial ahead of schedule, thanks to the engagement of our clinical site principal investigators and a truly outstanding manufacturing success rate at AIVITA.”
AV-GBM-1 is a novel immunotherapy consisting of autologous dendritic cells loaded with autologous tumor antigens. The treatment targets multiple antigens on the autologous tumor-initiating cells responsible for the rapid growth of the disease.