Wouldn’t it be amazing to be able to see a protein being made in a cell in real time? And wouldn’t it be even better if you could use that capability to discover new drugs to previously “undruggable” targets, creating new medicines? Well that’s exactly what Anima Biotech is aiming to do.
Wouldn’t it be amazing to be able to see a protein being made in a cell in real time? And wouldn’t it be even better if you could use that capability to discover new drugs to previously “undruggable” targets, creating new medicines? Well that’s exactly what Anima Biotech is aiming to do.
“We are going after mRNA translation to specifically target protein production using small molecules,” Yochi Slonim, co-founder and CEO of Anima, told BioSpace.
Anima’s technology uses state-of-the-art molecular biology that can illuminate the protein synthesis process and identify small molecules that regulate mRNA translation. They target proteins that regulate the translation process, which haven’t been targeted with drugs to date. This company aims to improve upon the rapidly growing RNA therapeutics area by addressing RNA as a therapeutic target differently and utilizing small molecules to improve upon some of the current therapeutics’ shortcomings.
Current mRNA-targeting therapeutics
Messenger RNA (mRNA) is the intermediate molecule between genes and proteins; it encodes instructions that are directly used to make proteins. It is a promising drug target because it offers another avenue to control protein production, rather than directly targeting the proteins. One way to alter protein production via RNA is using RNA interference (RNAi), where a small strand of RNA acts as the biological drug by binding to mRNA in a cell and preventing it’s translation into a protein. This process effectively knocks down the mRNA so that no protein is produced. Since RNAi was the topic of the 2006 Nobel Prize in Physiology or Medicine, RNAi research has exploded, especially in the biopharma industry. Unfortunately, this advance has been met with its own set of challenges, including serious and toxic side effects of some potential RNAi drugs.
The first RNAi drug, Alnylam Pharmaceuticals’ Onpattro (patisiran), was FDA-approved last August and it is showing long-term efficacy and sustained treatment for the rare disease hereditary transthyretin-mediated amyloidosis (hATTR amyloidosis). In addition to its fully stocked pipeline, Alnylam now has its eyes set on the next possible FDA approval, with the FDA granting priority review to their investigational RNAi drug for the rare disease acute hepatic porphyria, givosiran. As of March, Phase 3 trial data for givosiran is overall positive, despite some serious adverse events.
Silence Therapeutics, a UK- and Germany-based company, is also pursuing RNAi drugs for hematological, cardiovascular, and rare diseases. Its lead drug candidate, SLN124, is currently in clinical trials for two hematological diseases, beta thalassemia and myelodysplastic syndrome. Another candidate, SLN360, is currently in pre-clinical testing for cardiovascular disease, but is expected to move into clinical trials sometime next year.
Quark Pharmaceuticals is another RNAi company with its lead candidates currently in Phase 3 clinical studies: QPI-1002 for delayed graft function (a condition where a newly transplanted kidney does not work as it should, causing the recipient to still need dialysis), and QPI-1007 for non-arteritic anterior ischemic optic neuropathy (the sudden loss of blood flow to the optic nerve, which typically causes sudden vision loss in one eye without pain).
Another type of RNA therapy is to use the body’s own protein-encoding platform: mRNA. The idea is that, for diseases with a missing or mutated protein, the mRNA corresponding to the normal protein would be delivered into the cell using a virus or nanoparticle, where the mRNA would be translated into the normal protein using the cell’s own machinery. As straightforward as this seems, mRNA hasn’t come to fruition as a drug yet because it is highly immunogenic and highly prone to degradation not only in the cell, but once it is in contact with almost anything (enzymes that destroy RNA, called RNAses, are found almost everywhere).
Despite the difficulties of developing an mRNA therapeutic, there are multiple companies working in this space. Moderna Therapeutics’ lead drug candidate, AZD8601, is currently in a Phase 2 trial for myocardial ischemia (reduced blood flow to the heart). They also have multiple anti-viral and anti-cancer vaccines in Phase 1 trials. CureVac and BioNTech are also developing both anti-viral and anti-cancer vaccines. Translate Bio’s lead drug candidate, MRT5005, is in a Phase 1/2 trial for cystic fibrosis; whereas Arcturus Therapeutics and Ethris are both still at the pre-clinical development stage.
Although exciting advances in RNA drug discovery have been made in the recent years, RNAi and mRNA drugs have clinical hurdles to overcome that make them less than ideal drugs. The first is that, since they are biologic drugs made of genetic material (a double-stranded small interfering RNA (siRNA) in Onpattro’s case), they require a delivery vessel, like a virus or nanoparticle, to deliver the biologic drug into the cell. This means that the drug is not orally available, requiring an infusion to administer it to the patient.
Targeting mRNA translation with small molecules
Because Anima’s technology goes after the translation process, rather than the mRNA itself, it allows them to identify small molecule drugs that can impact protein production like an RNA therapeutic, but still have the pharmacological benefits of being a small molecule drug, such as being orally available. By targeting the previously “undruggable” proteins that control translation, it offers a new approach to controlling protein production.
A protein is considered “undruggable” when it is difficult or impossible to develop a drug that targets the protein using known drug development techniques. Novel techniques and drug classes are needed to address this unmet scientific need.
There are also some disheartening - or stimulating, if you’re up to the challenge of tackling this problem - figures out there. Up to 80% of protein targets are thought to be “undruggable” using the currently established classes of drugs and means of drug discovery. Another unfortunate figure is that, according to bioinformatics studies, less than 10% of all human proteins are expressed on the cell surface or secreted by the cell, meaning that about 90% are intracellular proteins that are harder to target. All of the currently approved drugs only target 2% of all human proteins, so many undrugged protein targets remain.
These figures highlight that current drug development techniques have fallen short in terms of targeting proteins. Not to mention that underlying biological understanding of disease pathology, as well as a drug’s mechanism of action, can be unknown, leading to more than 90% of new drugs failing. All of this leaves much to be desired and plenty of room for innovation.
Anima’s platform for targeting protein translation
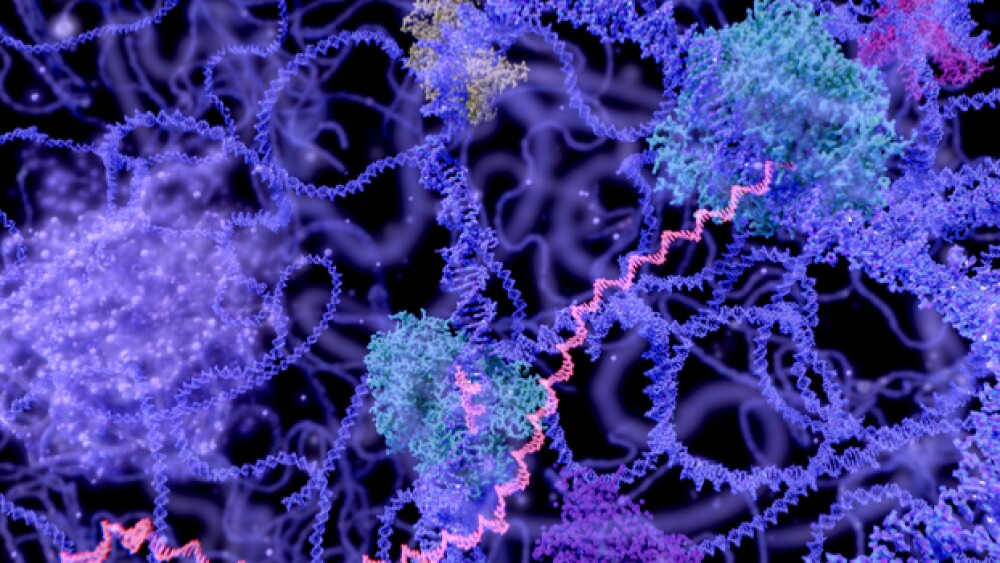
Using small molecules to control protein translation directly was not believed to be possible in the not-so-distant past. The advent of new technology, such as Anima’s Translation Control Discovery Platform, is now making this achievable. This platform allows identification of small molecules that modulate protein translation by binding to regulatory proteins that either directly interact with the mRNA, interact with RNA-binding proteins, or that regulate ribosome activity. Using this platform, the translation process can be visualized in real time, meaning you can actually get direct feedback of how a protein is being made from its mRNA template.
Before we get into how their technology works, let’s briefly review the translation process. A gene in DNA is transcribed into an mRNA sequence, which are the instructions for making the protein that the gene codes for. The mRNA sequence is broken down into 3-nucleotide segments (called codons), which each code for a specific amino acid. Transfer RNA (tRNA) molecules are what interact with the mRNA and bring the correct amino acid to the ribosome (the translation machinery responsible for turning the mRNA message into an amino acid code and eventually a fully formed protein). Each tRNA carries two things: a specific amino acid, and a 3-nucleotide segment that is complementary to the mRNA codon (called an anticodon), which allows the tRNA to recognize the right codon and bind to the mRNA. Then, with help from the ribosome, the amino acid is transferred from the tRNA onto the growing amino acid chain, which will fold up to become the protein encoded by the mRNA.
To visualize the translation process, Anima uses a special library of fluorophore-labeled tRNA molecules that are transfected into cells and can measure the special way they interact. Fluorescence resonance energy transfer (FRET) is a special interaction between two fluorophores (one donor fluorophore and one acceptor fluorophore) where they emit a unique wavelength of light only when they are close together. Therefore, light is only emitted when certain donor and emitter fluorophores, attached to tRNAs carrying specific amino acids, are right next to each other within the ribosome.
The frequency of these light-emitting pairs can be predicted based on the mRNA sequence of the protein; when two amino acids are next to each other, a light signal will be emitted during translation when their corresponding fluorophore-labeled tRNAs come next to each other. If there is a unique pair in a protein that repeats many times compared to the rest of the proteins in the cell, then this ‘signature pair’ of tRNAs provides a unique, detectable light signal that can be used to specifically track that protein’s production. Slonim said that 85% of proteins have these ‘signature pairs’ of tRNAs, allowing them to be tracked using Anima’s platform.
The intensity of the light pulses that these ‘signature pairs’ give off provide a way to specifically track a target protein’s synthesis in the cell; the more intense the light is, the more protein is being made and vice versa.
“Anima’s platform integrates image analysis and big data software where artificial intelligence identifies small molecules that increase or decrease the light signals,” said Slonim. “The molecules that change the light signal intensity are potential drugs that can modulate protein production by targeting the translation process.”
Baseline light intensity is established by looking at the protein of interest being made in cells with just the fluorophore-labeled tRNAs added. Then a library of small molecules is added to the cells in a high-throughput manner (one molecule per 5,000 cells in each well of a multi-well plate). The AI software program can then identify how each molecule effects the light signal: make it brighter (increase protein expression) or make it dimmer (decrease protein expression). Once a hit has been identified, the molecule’s impact on overall protein synthesis is analyzed and any molecule that interferes with protein translation in many cells or that target and affect the translation machinery itself is eliminated.
Understanding how these molecules affect protein synthesis can identify potentially novel drugs. Currently, Anima’s small molecule library includes around 200,000 diverse small molecules, consisting of FDA-approved molecules, licensed molecules from commercial sources, and new chemical entities.
“The AI software enables Anima to process large data from the molecule screens, but the real innovation lies in the ability to see translation biology in real time,” Slonim added.
This fully automated, high-throughput platform can not only be used to discover new drugs but can answer currently unanswered questions of how active compounds and current drugs actually work. Watching mRNA translation in action can also verify that the issue is in the translation (too little or too much protein being made) rather than the mRNA being truncated or possessing a premature stop codon to prevent the full protein from being synthesized.
Developing drugs and Anima’s pipeline
Anima’s technology not only allows for targeting the translation process directly, it also identifies drugs with two new capabilities: ones that can specifically increase or decrease protein production, and one that are potent, specific, and have little to no off-target effects.
Most current drugs can only regulate protein synthesis by inhibiting it. It is important to have drugs that can decrease (but not completely inhibit) or increase protein synthesis because different diseases may require up or down regulation of a protein to be therapeutically relevant. For example, Anima has identified compounds that either increase or decrease collagen production, both of which can be used in the wound healing and aesthetics industries.
Making sure the translation modulator drug is very specific is key; if a small molecule binds well to a protein involved with the target mRNA, it will bind to that protein anywhere in the body that the target mRNA is being expressed and translated. With no way to control the small molecule, there could be on-target systemic side effects from the drug indiscriminately binding the target protein outside of the particular organ or cell type of interest. For example, in lung fibrosis, you would want to selectively eliminate the collagen from the lungs, but no where else in the body, such as the skin or liver. Developing a drug specific for collagen produced in the lung sounds tricky (which it is), but the varying levels of protein expression in different tissues aids in the selectivity.
“Conventional drugs are like artillery,” Slonim told BioSpace. “These translation modulator small molecule drugs are like guided molecular missiles. This isn’t because they are ‘smart’ drugs, but it is due to their basic mechanism of action and the varied mechanisms regulating mRNA expression levels in different tissues.”
Anima is both developing their own drug discovery platform and partnering with pharma to screen against their targets of choice. They are targeting collagen in lung fibrosis with their lead compound and generating hits for two other collagen programs involved with liver fibrosis and scleroderma. Their next two lead compounds target RSV (specifically viral translation inhibitors) and C-Myc (involved in many types of cancer). Slonim also said they were making “huge progress” and had “encouraging results” developing a drug against an undisclosed target as a part of their partnership with Eli Lilly and Co.
C-Myc is an infamously “undruggable” oncoprotein in cancer, with its dysregulation being involved in more than half of all cancers and associated with worse patient outcomes. Although C-Myc represents a desirable target for cancer therapeutics, it’s “undruggable” structure has proven difficult in developing a drug against it. Anima’s translation platform allows them to see which small molecules selectively disrupt C-Myc translation in a dose-dependent manner.
Another target in the hit generation phase is huntingtin, which, when mutated, is a protein involved in Huntington’s disease. The diseased version of huntingtin is caused by a segment of the gene repeating many more times than normal: 36-120 repeats or more compared with 10-35 repeats in the normal protein. This abnormally long gene correlates to an abnormally long mRNA and eventually an abnormal protein, which can stick together and cause problems.
Using their platform, Anima can see the translation of the elongated mRNA in real time. They can then screen against a library of small molecules to find one that causes ribosomal stalling, where the ribosome stops translation of the mRNA at a certain spot before the end of the mRNA. Truncating the elongated mRNA sequence may restore normal huntingtin protein expression (with the normal number of repeated segments) by preventing the extra repeats from being added at the translation step, thus protecting against disease. This ribosomal stalling idea can be extended to any other disease with long repeats creating problematic proteins.
While Anima is still a pre-clinical company, they hope to get their lead compound in the clinic in about two years.